Barriers to surveillance for hepatocellular cancer among patients with chronic liver disease -providers' perspectives
Abstract
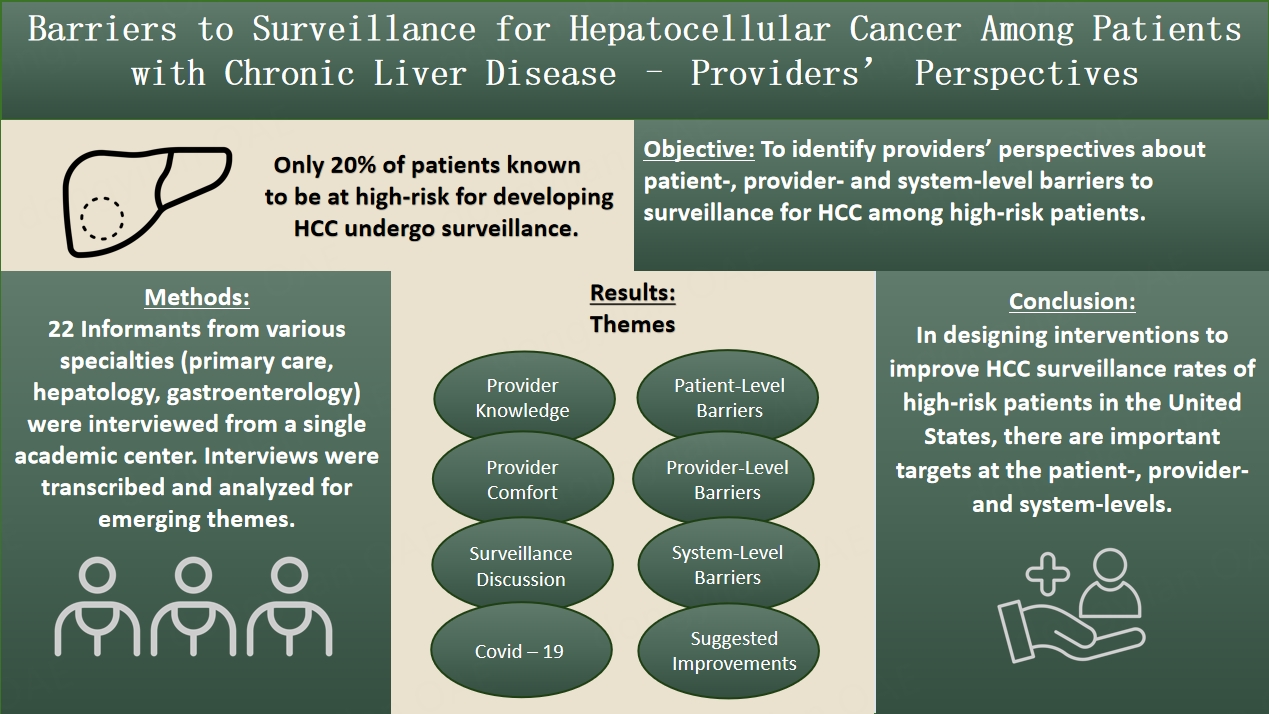
Aims: Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer. While patients who are known to be at high risk for HCC should be under surveillance, only 20% of eligible patients in the United States are surveilled. The aim of this study was to identify providers’ perspectives about patient-, provider- and system-level barriers to surveillance for HCC among high-risk patients and to examine provider knowledge and attitudes related to HCC surveillance. We also explored interventions providers suggested as ways to improve HCC surveillance.
Methods: Purposive sampling was used to recruit physicians and nurse practitioners in hepatology, gastroenterology, and primary care (internal and family medicine) from one academic medical center to participate in semi-structured interviews. Interviews were transcribed verbatim, and analyzed deductively and inductively to reveal emergent themes.
Results: 22 informants were interviewed. During these interviews, several important themes emerged, including: (1) Provider comfort with managing chronic liver disease and the relationships between hepatology, gastroenterology, infectious disease, and primary care providers; (2) Provider knowledge of guidelines for HCC surveillance in high-risk patients and their knowledge about the impact that HCC surveillance can have; (3) How providers discuss HCC surveillance with their high-risk patients; (4) Provider-Level barriers to surveillance; (5) System-level barriers to surveillance; (6) COVID-19; (7) Patient-level barriers to surveillance, and (8) Suggested interventions to improve HCC surveillance rates.
Conclusions: In designing interventions to improve HCC surveillance rates of high-risk patients in the United States, there are important targets at the patient, provider and system levels.
Keywords
INTRODUCTION
Hepatocellular carcinoma (HCC) is the fourth leading cause of cancer-related death worldwide - and the fastest-growing cause of cancer-related deaths in the United States (US)[1]. The prognosis is dismal - with only a 15% 5-year survival rate; however, patients diagnosed early are candidates for potentially curative therapies[2]. Most cases of HCC occur in patients with known risk factors for HCC, including chronic hepatitis B and cirrhosis from hepatitis B (HBV), hepatitis C (HCV), heavy alcohol use and non-alcoholic steatohepatitis, as well as other chronic liver diseases[2]. Studies have demonstrated that high-risk patients who undergo surveillance are diagnosed with earlier-stage HCC, are more likely to receive potentially curative treatment such as surgical resection or liver transplantation, and have improved survival in comparison with those patients who presented with associated symptoms or incidental detection of HCC and may only qualify for locoregional therapies and/or systemic treatment[3-5]. Therefore, expert society guidelines recommend HCC surveillance every 6 months for high-risk individuals[6-9]. Nonetheless, less than 20% of patients in the US with cirrhosis undergo routine surveillance[10].
Recent studies have also shown disparities in rates of surveillance, eligibility for surgical intervention, and survival in HCC patients with similar clinical characteristics in the United States[11-15]. Important barriers at the patient, provider and system levels have been identified. At the patient level, financial constraints, lack of awareness of scheduling recommendations, scheduling difficulties, and non-adherence were commonly demonstrated. Frequently identified provider-level barriers include a lack of provider awareness of surveillance guidelines, difficulty accessing specialty resources, order nonplacement, and time constraints in the clinic. System-level barriers commonly associated with poorer HCC surveillance included fewer clinic visits and rural/safety-net settings[16,17]. However, limited studies have been performed evaluating provider-reported barriers to HCC surveillance. In web-based surveys of primary care providers, providers identified not being up to date on HCC surveillance recommendations, difficulty communicating effectively with patients, limited time in the clinic, and competing clinical concerns as barriers to HCC surveillance[18,19]. Qualitative studies further exploring provider-reported barriers to surveillance have not been conducted. Additionally, specialists, including gastroenterologists and hepatologists, who commonly care for patients with cirrhosis, have not been included in prior research.
Therefore, the current qualitative study aimed to identify patient-, provider-, and system-level barriers to surveillance for HCC among high-risk patients from providers’ perspectives in the United States and to examine provider knowledge and attitudes related to HCC surveillance. Additionally, we explored interventions providers suggested that could improve HCC surveillance rates.
METHODS
Study design
Purposive recruitment was used to invite physicians and nurse practitioners from the Ohio State University Wexner Medical Center’s (OSUWMC) Departments of Internal Medicine and Family Medicine who provide primary care, and from the Department of Internal Medicine, Division of Gastroenterology, Hepatology and Nutrition who provide specialty care, via email to participate in qualitative interviews February-May, 2021. For the purpose of deidentification, hepatology physicians, hepatology nurse practitioners, and gastroenterologists are referred to as "specialists” and other providers as "primary care providers.” OSUWMC is an urban tertiary care center with approximately 1200 inpatient beds and 18 primary care sites in metropolitan Columbus, Ohio. Interested participants responded via email to schedule one-on-one virtual or in-person interviews with study team members. Participants provided written consent to be interviewed and have their interviews recorded. Interviews lasted between 9 and 27 minutes. Interviews were audio-recorded and transcribed verbatim.
Data collection
A semi-structured interview guide was used to ask providers about surveillance for HCC among high-risk patients, their knowledge and attitudes regarding surveillance for HCC, and opportunities to improve HCC surveillance. Provider knowledge and attitudes related to HCC surveillance were assessed using interview questions adopted from a survey by Dalton-Fitzgerald et al.[19].
Data analysis
Transcribed interviews were analyzed deductively and inductively to categorize our findings and reveal emergent themes[20-22]. The research team created a preliminary coding dictionary based on general topics covered in the semi-structured interview guide. The preliminary coding dictionary was then applied to three interview transcripts to confirm the applicability of the coding dictionary and begin to identify emergent themes that informed a refined and expanded coding dictionary. Members of the research team then used this revised coding dictionary to code the remaining transcripts, while meeting frequently to ensure consistent application of codes and review any new themes that emerged. Two research team members (EB, JV) coded all transcripts and examined coding to arrive at an agreement across all transcripts. ATLAS.ti 9, a qualitative analysis software, was used to facilitate the coding and qualitative analysis of the interview transcripts[23]. Additionally, descriptive statistics were calculated including proportions/percentages.
RESULTS
22 informants were interviewed, including hepatology and gastroenterology specialists (n = 10) and primary care providers (PCPs, n = 12). Informants spend a median of 70% (range 20%-100%) of their time in clinical practice, versus research and administrative responsibilities, and have been in practice a median of 7 years (range 1.8-25 years).
Several important themes emerged from interview data, including: (1) Provider comfort with managing chronic liver disease and the relationships between hepatology, gastroenterology, infectious disease, and primary care providers; (2) Provider knowledge of guidelines for HCC surveillance in high-risk patients and their knowledge about the impact that HCC surveillance can have; (3) How providers discuss HCC surveillance with their high-risk patients, 4) Provider-Level barriers to surveillance; (5) System-level barriers to surveillance, (6) COVID-19; (7) Patient-level barriers to surveillance; and (8) Suggested interventions to improve HCC surveillance rates.
Provider comfort with chronic liver disease and the relationship between hepatology and non-hepatology providers
Providers discussed their own comfort level, and specialists discussed which patients they continued to follow long-term, while PCPs discussed which patients they referred to hepatology [Table 1]. Specialists reported that they were comfortable managing patients with chronic liver disease and that they continued to follow a majority of patients with chronic liver disease indefinitely. Patients with acute liver disease or laboratory abnormalities such as elevated liver function tests may be referred back to their PCPs, but patients with chronic hepatitis B, chronic hepatitis C, and non-alcoholic fatty liver disease or steatohepatitis reportedly continued to follow with hepatology. One specialist stated, "Mostly following them long term. Occasionally, if I've answered the clinical question and their liver tests aren't bad, or you know, there are certain situations where I discharged them or, for example, if you identify Hep C, they don't have advanced scarring, and then you can discharge them after you cure the Hep C. But the majority I keep.”
The relationship between primary care and hepatology
| Quote | Provider type |
| “Those patients who have acute hepatitis, those patients who have abnormal liver function tests, okay, they usually go back to their primary care physician. Those who have chronic Hepatitis C treated successfully, those who have chronic Hepatitis B successfully on the antiviral therapy, so they actually are referred back to their primary physicians” | Specialist |
| “Yeah, so the kinds of reasons why I might refer them [to a hepatologist] would be, for example, if I, this happened just recently, incidentally pick up a chronic viral hepatitis. Or I would refer them if I, if they have fatty liver disease and I'm concerned about the degree of fibrosis” | Specialist |
| “For the most part, I'll do their HCC screening and then if they need screening esophagogastroduodenoscopy, I will order those as well. So, I can do it if it's uncomplicated. But if they're, you know, definitely they have decompensated cirrhosis, then I try to push them over to hepatology to co-manage” | Primary Care Provider |
| “When I first started and there weren't therapies and somebody has chronic Hepatitis C, I was able to, you know, do the hepatocellular carcinoma screening and some of the other monitoring myself. But since there have been therapies for Hepatitis C, I have definitely referred to hepatology for that. And then I think, you know, same with non-alcoholic fatty liver disease, I do refer to hepatology. Especially if my patients have evidence of chronic hepatitis, they're not responding to lifestyle measures, but I would say that I don't necessarily refer every single patient” | Primary Care Provider |
| “No, I do think that having a great hepatology department here and like I said, like the new, having the E-consults where we just have a way to ask some questions, to review labs, imaging and sort of having the specialists give us the most up to date recommendations or even just their expert opinion if it for some reason falls outside of the guidelines, it has been super useful” | Primary Care Provider |
| “If they have cirrhosis, I will. If I just know that they have like some sort of like hepatic steatosis or something like that and their LFTs aren't like super high, then I'll just continue to monitor. I may get like elastography myself or I may, sometimes I also because hepatology now has E-consults, I may E-consult them for recommendations and most of the time with them saying, hey, make sure you get your hep panel and your elastography in addition to your ultrasounds and if it gets worse then we’ll send them to hepatology” | Primary Care Provider |
| “Once I know they’re higher risk, I feel better having them see a specialist just because I don't know all the nuances and I don't stay up to date on all the research. You know as recommendations change” | Primary Care Provider |
| “So if it’s fatty liver you know I typically start the initial workup, so if we find that through imaging, we’ll follow them with monitoring tests. Repeat right upper quadrant ultrasound, pursuing fibro scan if necessary, appropriate, focusing on dietary modifications, medication management, trying to get chronic things such as diabetes/hypertension under control. If things are progressing or we find it is progressive, absolutely put in a referral to hepatology” | Primary Care Provider |
PCPs reported varying comfort levels taking care of patients with chronic liver disease, ranging from "Not comfortable” to "Fairly comfortable” and variable indications to refer such patients to hepatology. One PCP stated, "I generally do the labs, and the right upper quadrant ultrasound, and if I see fatty liver, I do transplant elastography and if it comes back showing higher risk, then I refer them on.” PCPs reported a good relationship with hepatology and clear and easy communication, especially with the introduction of an electronic consult process, where the provider can ask hepatology a specific question about a patient without the patient having to see hepatology. One PCP stated, "Yeah, it's really easy to get people in and I get clear communication back. And so it's very clear what needs to happen next. And a lot of times in the future, I'll order all the stuff ahead of time before the patient goes to their appointment, just to make things a lot easier for them.”
Provider beliefs about which provider is responsible for HCC surveillance varied [Table 2]. PCPs most commonly reported that the responsibility for HCC surveillance in high-risk patients is shared between PCPs and specialists. One PCP stated, "I think it needs to be a shared thing. If the patient is only with primary care, the primary care provider has to keep and has to take ownership of the patient. But if hepatology is following along, then I expect them to also like to make sure that the patient is following up on their screenings.”
Which type of provider is responsible for HCC surveillance?
| Category | Quote | Provider type |
| Combined responsibility | “I think there's a shared responsibility. Especially if a patient is seeing both the specialists and primary care” | Primary Care Provider |
| “I say all of the above. Understanding that there's a large portion of patients who may not be able to get in to see a gastroenterologist/hepatologist and are primarily under the care of their local PCP” | Specialist | |
| “I think primary care providers definitely can be involved. I think hepatologists would be involved. And then I think infectious disease should be involved as well. Sometimes it's a little, there's some overlap when we share patients with hepatology. It can be a little bit confusing who's responsible for it. But for the patients that are not seeing hepatology, then I do think it's our responsibility” | Primary Care Provider | |
| Hepatologist responsible | “Well, we all have responsibilities. But if the patient is seeing a hepatologist, it’s primarily his responsibility. But if the patient doesn't have access to a hepatologist or gastroenterologist, then I think a primary care physician needs to step in and do that job” | Specialist |
| “I definitely think it should be a specialist and I think you should be managed by a specialist. But under the umbrella care obviously of having a family doctor. You can't do everything as a specialist, but I also think you can't do everything as a primary care” | Specialist | |
| Depends on situation | “If you’re at a large academic medical center like myself. You know you have very easy access to hepatology and once you get those baseline imaging studies, baseline labs and you're referring for further evaluation and management, you know, I might say it's the specialist’s responsibility. So I think it's dependent really upon your practice location, your practice populations, and resources that are available to you. You have to take that into consideration when you're trying to lay blame or responsibility” | Primary Care Provider |
| “It depends on if they're the primary care provider who is capable. I think he can easily do screening like the way they screen for prostate cancer. They screen for colorectal cancer” | Specialist |
The majority of specialists reported believing that HCC surveillance is the primary responsibility of a patient’s hepatology team. One specialist stated, "I honestly do think it should be hepatologist because I think that, you know, someone has cirrhosis, they should follow them long term in a hepatology clinic...that sort of contact, I think, is very important because you're also not just looking at cirrhosis, you're looking at screening for varices, so many other things that again I think a yearly visit with someone in hepatology clinic or GI.” Another specialist acknowledged that it depended on the patient’s access to care, "That can really depend on where the patient is. We are so fortunate because we actually have hepatologists and I can say I don't do liver. But even in the community, most gastroenterologists couldn't say that. And then if you get further away, patients may not have access to even a gastroenterologist, much less a hepatologist.”
How providers discuss HCC with their patients
All provider types reported discussing HCC surveillance with their high-risk patients in varying levels of detail [Table 3]. One specialist reflected, "Every time I talk to them, I try to make them realize the importance of surveillance. I always tell them that the reason is to actually screen for HCC and diagnose it early, because early diagnosis is the key to successful treatment. We give them a booklet about cirrhosis and its different complications and screening tests. And I do actually add in the AVS [After Visit Summary] about the information on their HCC screening." One PCP commented, "Well, I talked to them that you would be in an at-risk category; definitely having more knowledge is better than not enough so that we can make good choices in terms of your options. I mean, just because we find it doesn't necessarily mean we have to do something about it. But having that knowledge helps us give you better options to make better choices."
How providers discuss HCC surveillance with their patients
| Quote | Provider type |
| "I really spend a lot of time explaining how important it is. And that they will not have symptoms related to cancer until it’s very late. So, it's extremely important for us to catch it early" | Specialist |
| "After I make the diagnosis of cirrhosis, I tell them a little bit about pathogenesis that it can, depending on what stage they are, it can progress to liver failure or liver cancer both as a complication and I give them a printed handout of cirrhosis, with its potential complications listed. And then, I emphasize the need for diagnostic surveillance and screening, especially for liver cancer. So, a lot of times, they feel that the ultrasound is being ordered to check on the status of their cirrhosis. I said, no, that's not the reason. We are doing it to screen you for liver cancer specifically. And it needs to be done every six months because if we don't catch it and we catch it in the late stages, the options become very limited. But if we catch it early, you have quite a few options in terms of treatment and surgery" | Specialist |
| "I’ll tell them due to your underlying liver disease, you're at a risk for developing liver cancer. So, stress the importance of doing these imaging modalities at least every six months" | Specialist |
| "Yeah, I think, especially since I was a nurse first, education to me is huge. So, I probably spend way too much time with my patients. But a lot of it is because I'm educating. I'm not just throwing information at them, I’m making sure they understand it so that they can repeat it back to me. At the end of the visit, we summarize together what our plan is and then I make sure I give them patient instructions in regards to that. So that way, it's very clearly detailed. So, I think health literacy and that part is really important to me. So, I try to always make sure I spend extra time on that" | Specialist |
| "I guess I don't really use those words. It's just kind of like, the wrapped up in the things that we do. I don't know. You know, like, like labs and ultrasounds. So, it’s, and I mentioned that more than one of these blood tests is to check for liver cancer. But I don't know if I’ll necessarily highlight it there" | Primary care provider |
| "Yeah, I just say because they have increased risk of developing liver cancer like HCC and then say that potentially could be cured with transplant or you know, other, it could be treated if caught" | Primary care provider |
| "It's just like hey, you owe me an ultrasound... Because like some of these, you know, they've made the decision that like they don't want to go to the hepatologist anymore, they want to follow with me. And so like, it's like, so it's kind of like that gives me a little leverage. Like dude, if you want me to do this, you gotta, you gotta meet me, you know, this is what I'm recommending" | Primary care provider |
| "I guess I would use the classic kind of terminology that if we find something early, then there's more options to treat. And that's why we want to screen. I think I would use that kind of language, but I don't have any other script. I don't have a complex script for that, you know" | Primary care provider |
| "I try to take patient preferences into consideration in any medical decision and I don't think HCC screening is any different. You know, usually, I will kindly talk to patients about my recommendation and, as I mentioned, kind of the pros and cons of HCC screening, or if it was recommended by their hepatologist, I will let them know that. And then, I do listen to their preferences, ask them if they're okay with proceeding with us, if they have any concerns about the testing. And, and we go from there" | Primary care provider |
Provider knowledge of guidelines and outcomes from HCC surveillance
Providers reported varying levels of familiarity with guidelines for HCC surveillance [Table 4]. Specialists most commonly reported using the American Association for the Study of Liver Diseases (AASLD) Guidelines and several reported being involved in updating the guidelines, reviewing the guidelines regularly and being able to summarize the guidelines. One specialist stated, "So, [for] all the patients with cirrhosis particularly, I follow the AASLD guidelines. So all the patients with cirrhosis, all the patients with Hepatitis B virus infection.”
Provider knowledge of guidelines for HCC surveillance
| Source | Specific guideline used | Involved in updating guidelines | Review updates regularly | Can summarize guidelines |
| Specialist | AASLD | No | Yes | Yes |
| Specialist | AASLD | Yes | Yes | Yes |
| Specialist | AASLD | Yes | Yes | Yes |
| Specialist | AASLD | No | Yes | Yes |
| Specialist | AASLD | No | Yes | Yes |
| Specialist | AASLD | No | Yes | Yes |
| Specialist | AASLD | No | Yes | Yes |
| Specialist | Not sure | No | No | Yes |
| Specialist | AASLD | No | Yes | Yes |
| Specialist | AASLD | No | Yes | Yes |
| Primary care provider | Not Sure | No | Yes | Yes |
| Primary care provider | AASLD | No | Yes | Yes |
| Primary care provider | Not sure | No | No | No |
| Primary care provider | AASLD | No | Yes | Yes |
| Primary care provider | AASLD | No | Yes | Yes |
| Primary care provider | Not sure | No | No | No |
| Primary care provider | Up-to-date | No | Yes | No |
| Primary care provider | Not sure | No | No | No |
| Primary care provider | Not sure | No | No | No |
| Primary care provider | Not sure | No | No | No |
| Primary care provider | Not sure | No | No | No |
| Primary care provider | AASLD | No | No | No |
Provider-level barriers to surveillance
Several provider-level barriers were identified, including (1) knowledge; (2) time in the clinic; (3) competing issues in the clinic; and (4) deferral of responsibility [Table 5]. With respect to provider knowledge, one PCP noted, "The other thing is, I'm just maybe this is going to come up, but like, I'm always like, well, who gets an ultrasound? Who gets an MRI? Who gets a fibro scan? Who gets a? Yeah, that's where I get kind of confused. I'm like okay, I just follow whatever they said to do, but I'm like, I'm not sure…Clearly, I’m identifying a knowledge gap in my own practice." Providers also identified time in the clinic as a provider-level barrier to HCC surveillance, with one PCP reporting, "Your schedule, patient load, and if you only have 20 min with patients coming in to see you for what is important to them. If you go into the room thinking, okay, I'm going to go over this, this, and this. The patient is there for something that they're concerned about that has nothing to do with your list. You may end up having to follow up with them on that at another time.” Competing issues in the clinic were also noted to be an important barrier, with a PCP stating, "I think, at least for primary care providers, a lot of patients have a lot of things going on, so I can see how it can be pushed under the radar as a less urgent issue. And then every six months is actually, you know, pretty frequent screening." Deferral of responsibility, or not knowing what type of provider is taking responsibility, can also be a barrier, with one PCP reporting, "I don't know if a lot of doctors, a lot of like primary care doctors see it within the scope of their practice. And so, they'll just like, refer, like offload, all of that to infectious disease or hepatology."
Provider-Level Barriers
| Provider – provider knowledge | "In the primary care setting, I think there's just so many different guidelines things that you're trying to stay up to date with and so, sometimes, I think that can be challenging...I was going to say lack of knowledge" | Primary care provider |
| "I think probably one of the biggest barriers would be a barrier in terms of knowledge. In terms of what's recommended, why, or what impact or difference it can make...Right so, I think a lot of times it can be, you know, really knowledge barrier on the part of the provider in terms of kind of buying in. Knowing, you know what the recommendations are and buying into the importance of why we want to do it" | Specialist | |
| "Knowing what to do with a positive screening test. Kind of where that next step is. So, I think again, you know, we're so privileged, because you know, we have hepatologists, and we have surgeons and we have this huge support network with our radiologists basically telling us what to order next, you know. But I don't know that that's necessarily a luxury that everyone enjoys. So, I think knowing maybe the next steps would also be helpful for providers who are trying to provide the best care for patients" | Specialist | |
| Provider - time in clinic | "Definitely, on like some of those patients I talked to, I'm trying to educate them and convince them, like if they're really reticent, but if I had like half an hour to an hour more to discuss with them, maybe I could convince them. So, definitely timing" | Primary Care Provider |
| "So in my, so my view would be that if they haven't done surveillance done, it is either because it hasn't been brought up by the person who's managing their liver disease, whether that's hepatology, GI, or primary care. So, that may be a lack of awareness, you know, nobody's really talked to them about it" | Specialist | |
| "Insufficient time in the clinic" | Primary Care Provider | |
| Provider – competing issues in clinic | "I sometimes have to prioritize what I can address and, you know, especially if they have an urgent concern or disease exacerbations. I think that just trying to figure out how do you address everything, including HCC screening, which is more of a kind of anticipatory intervention rather than putting out a fire" | Primary Care Provider |
| "Often. And those competing interests can be different. Usually, it's a patient will come in with 10 things that are not related to surveillance and so those are competing interests. So are we going to focus on the list of what patient brings in, or are we going to focus on health maintenance today? And those are, there's a lot of competing interests with that almost every time" | Primary Care Provider | |
| "Competing interests in the clinic" | Primary Care Provider | |
| Provider - responsibility deferral | "They're shouldn’t, I mean, it's pretty easy, right? Not that I know of, no" | Specialist |
| "I would say I think it's probably easy to think if someone is seeing hepatology that like hepatology will take care of that...I think that so kind of lack of clear responsibility" | Primary Care Provider | |
| "Assuming that someone else is monitoring it or following it" | Primary Care Provider |
System-level barriers to surveillance
System-level barriers identified included: (1) The absence of technology tools; (2) insurance denial of surveillance imaging; and (3) difficulty scheduling surveillance studies (Data not shown). The most commonly reported system-level barrier was the absence of technology tools. Overall, providers reported that there are no technology tools such as order sets, best practice alerts, reports or reminders in the health maintenance tab built into the electronic health record that they use to help with HCC surveillance. One provider stated, "I don't use any order sets and I don't have any pop-up best practice alerts.” On the other hand, some providers did report having a portion about HCC surveillance built into their own note templates, "I have a cirrhosis template and the HCC screening recommendation comes up as part of my plan,” or personal smartphrases that they use, "I do have a Dot phrase that I use. I wouldn't say I use it for everyone, but it's sort of something that, at least in my patients who have cirrhosis that, you know, makes me alert to it or at least think about it.” With respect to insurance, one provider stated: "Sometimes insurance questioning surveillance. You know, we just peer-to-peer and fight for it as much as we can.” With respect to scheduling surveillance tests, one provider stated, "The barriers, I think, also with the scheduling for the ultrasound, of course, can be improved upon. I think if there's maybe a little quicker and getting the patients called and scheduled, it's something that after they leave the office visit, we just talked about so it's fresh in their mind. But then if a week or so goes past, they don't hear anything, then it can get lost and they don't call to schedule it or something like that.”
COVID-19
Providers reported that COVID-19 has impacted surveillance for HCC in the following ways [Table 6]: delayed surveillance secondary to fear of nosocomial infection and follow-up scheduling obstacles secondary to patient encounter modality shifts, such as the shift to increased TeleHealth visits and increased use of patient portals. In response to whether COVID-19 had been a barrier to surveillance, a provider responded, "I am sure. I hear from my patients, actually, stories that they are unable to get blood testing because of COVID-19. They are scared to go to the laboratory. They give the same explanation when they are unable to get the ultrasound as well. People are actually scared going to the facilities.”
COVID-19 impact on HCC surveillance
| "I will say I've had several people decline HCC screening within the past year because they don't want to come into the hospital because of COVID-19" |
| "I feel like things that have been tricky is scheduling for sure, especially with like doing Telehealth visits. The scheduling component for sure and then the fear of going inside the hospital. So I think some people were delayed this last year because of that…And I think that was just fear to come into the hospital because of the pandemic" |
| "I will say that COVID-19 has impacted across the board...I think mostly because people are not coming into the office or they're just foregoing medical care all together" |
| "I think that specific to the pandemic, we've had some barriers just trying to figure out the flow of Telehealth, making sure these patients are, you know, getting in touch with us. And also, I think some of my patients have told me too that they've missed a lot more appointments" |
Patient-level barriers to surveillance
Providers discuss several important patient-level barriers to surveillance for HCC [Table 7], including transportation, travel distance, scheduling difficulties, distrust of the medical community, lack of compliance, language barriers, busy life obligations, barriers to time off work, inadequate support system, poor coordination with local centers, religious fatalism, continued substance abuse, and health literacy. When discussing patient-level barriers to screening, one provider responded, "A lot of times, patients have difficulty with digital literacy, language barriers, especially my patients. Or they don't speak, they don't all speak English. And location or drive. So, if I get them to agree to go to do the screening, from their standpoint, there is the problem of, oh gosh, this is so far from my house. This is so far from where I live,” emphasizing transportation and travel distance as important barriers to surveillance. Providers also reported that health literacy was a relevant consideration regarding HCC surveillance. In response to whether health literacy impacted patient care, one provider responded, "100%. Not only on this matter, but in every matter. But certainly, the screening is probably the most likely affected and impacted by the lack of literacy in our population. I mean, in general, the basic proficiency in health literacy is less than 15 percent in the U.S. American population in general. And if you were to break it down by minorities and underrepresented communities, the disparity would be shocking and disappointing at the same time. So, I don't necessarily think that screening is, of HCC, is only one impacted. But certainly comes at the bottom of the list because it's not also like marketed as others.”
Patient-level barriers
| Barrier category | Quote |
| Transportation | "Transportation. I think transportation is huge. And then just having people find the time to come to the hospital" |
| "Well, yeah, just in general for my patient population, any time you're doing anything outside of that office visit, it's going to be more challenging. Especially if they have, a lot of my patients, they would be candidates for screening. Transportation is a huge barrier" | |
| "Transportation is a huge issue because patients need to have someone who can take them. And a lot of patients don't have somebody who can take them. Either they are a caregiver for someone and so they can't. Or they just don't have someone who can take them during the day" | |
| Distance | "…If I get them to agree to go to do the screening, from their standpoint, there is the problem of, oh gosh, this is so far from my house. This is so far from where I live" |
| "Distance is a barrier definitely. They’re reluctant to come 2 h away, 3 h away in bad weather just to get an ultrasound. So, we try to work with them and get them arranged locally or we try to coincide with their next appointment which could be with any other specialties, so they don't have to make a separate trip" | |
| Insurance | "I've had to do peer-to-peer reviews with these insurance doctors who may be orthopedic surgeons and trying to decline a hepatologist’s recommendation that patient needs CT or MRI" |
| "So, for a specific group of patient, I believe that the guideline must change about the screening for HCC because when we actually start the process of screening these patients with the help of CT scan or MRI, we find a lot of barriers in the form of approval from the insurance" | |
| "Well so I have had patients decline screening, saying that it was just around insurance coverage. So, if somebody has a really high deductible plan, and they'll say well you know, I haven't met my deductible this year, can we defer this?" | |
| Difficulty scheduling imaging tests | "The barriers, I think, also with the scheduling for the ultrasound, of course, can be improved upon. I think if there's maybe a little quicker and getting the patients called and scheduled, it's something that after they leave the office visit, we just talked about, so it's fresh in their mind. But then if a week or so goes past, they don't hear anything, then it can get lost and they don't call to schedule it or something like that" |
| "A lot of times, they forgot to schedule it, or they had to change it...It's a lot of times, they just go like oh, I didn't schedule it or no one followed up with me on scheduling it" | |
| "Yeah, a lot of times if they got busy. They had to cancel their test, they forgot to reschedule it...I think usually it's just scheduling-wise getting in the way, things getting busy" | |
| Distrust of the medical community | "...There is definitely a large proportion of patients who also have some mild distrust of the medical community in general. I think that plays a part, so that might be part of it as well or even just poor understanding of their own healthcare despite our best efforts at trying to educate" |
| "One is mistrust in the healthcare system. They feel like insurance companies are always trying to get their money. That's almost like a constant discussion of my patients" | |
| "They don't necessarily trust the provider. So, I'm not really sure that the provider-patient relationship is a factor that could be specific to hepatocellular carcinoma. I think it should probably be reflected in the global health of a whole person. So, I don't necessarily feel like you would even get to that discussion if you don't have a good provider-patient relationship" | |
| Lack of interest/compliance/knowledge | "And if the patient has to navigate screening modality for asymptomatic pathology, they're not going to do it. They don't have any incentive to do it. So I can give them the number every time they come in, I can send it through MyChart message. But if we want it to happen, navigating this monstrous system, you probably want to work with a referral specialist to call and say hey, we can schedule you in a place close to your home on a date that is convenient for you. Would you approve? Yes, that’s called partnership with the patients where they are empowered and enabled to approach the screening piece" |
| "It would be more a lack of compliance" | |
| "And then if patients aren’t invested in it, or they don’t see the relevance or the importance, they’re not going to get the test scheduled. They aren’t going to show up to those appointments. They aren’t going to follow up" | |
| Language barrier | "So that's or like, there's some kind of like language barrier. So, there's a couple of the factors of all kinds that affect patient's decision" |
| "I don't know if it's like a language barrier or education, but I will have patients that come back that I have done nothing. That I mean haven't even gotten a lab and they want to know how they're doing. Then I'm like you didn't do anything I asked. So I, and I don't know sometimes if that is a language thing because I do find that the majority of my Hepatitis B patients use English as a second language. So, you know, it's whether that's the barrier or if it's just not following through might just be what they do" | |
| Life is busy | "If people get busy that they may not have like a follow up regularly, then the patient's made lost a follow-up and then they returned as a with the new, with the new lesion in the liver" |
| "You know, they're busy, they forgot” | |
| "A lot of times if [patients] got busy. They had to cancel their test, they forgot to reschedule it...I think, usually, it's just scheduling-wise getting in the way, things getting busy" | |
| Getting time off work | "I think with, especially with our specific patient populations around here, you know, scheduling, timing and then transportation can always be difficult, because you know…a lot of our patients are working class and it’s sometimes difficult for them to take time off to begin with, but some many others also have significant transportation issues" |
| Support System | "...especially the people who are elderly, who have multiple other medical conditions, or they don't have good like a social support and their families are not around...factors of all kinds that affect patient's decision" |
| Coordination with local centers | "I know that the quality of the ultrasound is not very good in the local centers. Okay, and quite often, they miss actually even cirrhosis, leave aside the diagnosis of HCC, but I do allow them to actually go ahead and get done from their local centers" |
| "There’s patients who come from two hours away. For example, then you have to try and coordinate their ultrasound locally, at their local facility and that can sometimes be a barrier itself. And ultrasound may be done, but the report may not always get transmitted to me. So, you have to track it down, or when you see them next time, you find out that ultrasound was done locally" | |
| Religious fatalism | "They feel like you know religious fatalism, I think. I have a lot of faith-oriented patients and that is like one of their prognostic factors. So, they tend if, you know, if God's will, I will have the cancer and if God's will, I will die. So, the screening, in general, as a concept, is negated in that population. Luckily, I'm able to navigate that also using faith-based tailored counseling" |
| Continued substance abuse | "Low health literacy, inability to maintain appointments on a regular basis for lots of things, ongoing substance abuse. You know, you name it. Could be any and all of those" |
| Health literacy | "I think that just in general, health literacy probably affects cancer screening in general" |
| "I do think, again, if we did a better job maybe informing them about the risks of the HCC, they would be more apt to get it done if they fully understood what we're looking for and why it matters" | |
| "...when people don't follow the instruction for our recommendation for surveillance...sometimes it's just because they don't, they don't understand why" |
Suggestions to improve HCC surveillance
Providers had many suggestions to improve HCC surveillance [Table 8], including improving patient education, improving provider education, mass media campaigns, improving the use of technology tools, introducing patient navigators, increasing hepatology and primary care collaboration, and including recommendations for surveillance in radiology reports. With respect to patient education, one provider stated, "Educating the patients more. Taking more time on it because, again, it's not something that I necessarily spend a whole lot of time talking about when there are other things going on too. "Providers also suggested improving provider education,” "I think it's just education. I don't feel like providers would be resistant to doing something that has this proven benefit for the patient and for survival rates. I think then it's kind of more like spreading the word, getting the word out there of this is what's nationally recommended and you know, it's evidence-based best practice." Providers also suggested mass media campaigns, "You have mass media campaigns about lung cancer, breast cancer, colon cancer. There is a colon cancer month. There's nothing that is dedicated to liver cancer. So, I think that's where we need a national campaign actually, if you want to make an impact in reducing incidence as well as mortality. I mean, half of the patients who have liver disease, half of the patients who have Hepatitis C, don't even know about it."
Suggestions to Improve HCC Surveillance
| Suggested intervention type | Quotation |
| Patient education | "I think definitely doing more like patient education around it...if you had some patient education that was tied to like the diagnosis or if you just gave them information via MyChart, I think that would be potentially helpful because that would take some of that barrier off of like the provider having to go in and you know, add specific education all the time" |
| "I think it's more education. You know, I'm very specific about it, but you know, I know a lot of other people are not. Just like, "oh my livers getting checked out with an ultrasound," but they don't know why. Like they are looking to see like how well their liver is functioning. You know, I think it's just a lot of upfront education" | |
| Provider education | "I think that primary care physicians, for some reason, their attention span has become short, like all the adult population. They tend to work very well with algorithms...I think algorithms for providers. And then, honestly, you need to preach the media" |
| "I think it would be helpful to have just kind of a whether it be a grand rounds type of thing, or some kind of educational piece updates on hepatocellular carcinoma screening for primary care or just in general then having some of those guidelines for screening criteria. Just make it more, increase awareness, I guess through doing something like that. If there's a good flow chart, like a decision-making flow chart, those are always helpful. Having like a reminder pop up on the health maintenance thing in MyChart" | |
| Mass media campaigns | "So, I think if the, at least American Board of Family Medicine or American Board of Internal Medicine can actually, or even the GI Society can actually invest in some sort of a commercial. With the social media platform, we can reach out to a wider population. And they probably need to diversify as well their, you know, their recruits in order to improve screening amongst all minoritized communities" |
| "You know, a few years ago, when they did that big campaign for everybody over 50 to get Hepatitis C testing, there were billboards up on the interstate. If your, if your birthday is over such and such or before such and such you need to get checked for Hepatitis C. So obviously, social media has a huge impact on patients and patient care. I've realized my patients are much more likely to do something if they saw it on TV, or if it was out there, my patients are all about social media. But I do think from a system level, if we want to have increased screening, I think people need to know about it and need to know about the risks and why it's important" | |
| Technology tools - health maintenance tab | "In terms of our health maintenance tab, I think that tab could be a lot more functional for a lot of different things ... I think that would be super useful" |
| "I mentioned kind of being able to have some type of alert built into the health maintenance tab similar to diabetes. So, I think that could be, that could be really helpful" | |
| "It could be added to our health maintenance for certain diagnosis. Whether we add it, or hepatology adds it, for instance. You know, if there's a way to add needs yearly screening. That would certainly, I mean, I certainly look at those every time the patient is in the health maintenance tab" | |
| Technology tools - best practice alerts | "I think that thing that pops up and says they are due for a flu shot could say they are due for HCC screening" |
| "I think it works best when the system looks at the problem list and history. And if it identifies cirrhosis, chronic liver disease, fatty liver disease, you know, like all the diagnoses. Then, it can trigger an alert if the patient hasn't had a right upper quadrant ultrasound within the past six months. And you know, I would say that it should, it should go off if you're seeing a primary care doctor or the gastroenterologist. I wouldn't do it for just anyone though, because that, that's overwhelming" | |
| "I think if you had, you know, if it came up at least with Epic, if you know, if it came up as a reminder to the provider or to the patient hey, you’re due for your HCC screening, I think that would be helpful" | |
| "While I loathe the recurrent pop up, occasionally having the, you know, something like that is effective" | |
| Patient Navigators | "So, we have a navigator. We're fortunate to have a patient navigator on our team and that navigator keeps a spreadsheet so that we're following people both from a surveillance standpoint" |
| "Yeah, you could do like a patient navigator for people that are high-risk to help them with identifying barriers. You can also do like a peer navigator potentially. I think for like transplant and like oncology and things like that you, they have navigators. We’re trying to develop it for other like chronic conditions like HIV having a patient navigator to help patients remain in care and help them address barriers to keep them in care" | |
| Increased Hepatology and Primary Care Collaboration | "Potentially, if there was a way to increase collaboration with hepatology. I don't know what that would look like necessarily" |
| "It's just having that subspecialty experience around the community. It's the education of those docs in the surrounding area to provide more education to community providers about when to refer and who is at risk" | |
| Recommendation for Surveillance in Radiology Reports | "Let me think, anything that’s patient-centered. Potentially, if you put it in like radiology reports. Like if someone had cirrhosis, if they just added that to their dictation 'consider, chronic hepatitis or HCC screening'" |
DISCUSSION
Providers in our study reported important provider-level, system-level, and patient-level barriers to HCC surveillance that should be considered when designing interventions to address the low rate of surveillance among high-risk patients in the United States. At the provider level, providers identified their own lack of knowledge, limited time in the clinic, competing issues in the clinic, and deferral of responsibility as important barriers. These are consistent with prior surveys of PCPs in which it was identified that PCPs reported not being up to date on guidelines and having limited time in the clinic and competing concerns as barriers to HCC surveillance[18,19].
Notably, the specialists we interviewed noted that they continued to follow patients with chronic liver disease indefinitely and reported that they felt that HCC surveillance was their responsibility. Given that, to our knowledge, this is the first qualitative study to include specialists, this is a new and important finding.
PCPs we interviewed noted that most of their patients with chronic liver disease follow with hepatology. This finding is consistent with prior studies. In a qualitative study of 24 PCPs from seven Veterans Affairs facilities, PCPs reported that while they brought important skills to bear in the management of patients with cirrhosis, they preferred to defer major cirrhosis management decisions to specialists[24]. Given the current and future shortage of hepatology providers, which may disproportionately affect parts of the United States that are medically underserved, it will be important to target future interventions that include PCP education to improve PCP comfort in managing patients with cirrhosis, including comfort with surveillance for HCC[25,26].
At the system level, providers noted that there are not currently EHR-embedded resources such as order sets, best practice alerts, or health maintenance tab entries to support HCC surveillance. Although few studies discuss current EHR resources in use for aiding in this surveillance, many authors suggest leveraging technology tools with best practice alerts or integrated artificial intelligence algorithms to improve HCC surveillance through the identification of appropriate patients and provider prompting[27]. This type of intervention approach was also suggested by providers in our study.
The impact of COVID-19 was also noted. Evaluation of global trends for surveillance at three medical centers in the United States, Singapore, and Japan revealed that clinic visits, surveillance, and diagnostic imaging decreased dramatically secondary to measures implemented during the COVID-19 pandemic[28]. COVID-19 imposed surveillance limitations on many types of cancer, including gynecologic and colorectal[29,30]. A 65.2% decrease in the incidence of all new cancers in April of 2020 was reported secondary to screening deficits at the height of the pandemic, as evidenced by a study utilizing a platform of 20 U.S.-based institutions with relevant, up to date data with a patient population accounting greater than 28 million[31,32]. A reduction in surveillance for HCC has also been reported[33-35]. Interestingly, some studies have pursued strategies to optimize surveillance for high-risk patients with chronic hepatitis B utilizing antiviral therapy, including recommendations for using the modified REACH-B score, a risk prediction model for HCC[33,36] and other sources have recommended prioritizing surveillance for patients waitlisted for LT and reasonably extending the interval of surveillance for patients with lower risk tumor features as a means to limit patient exposure to COVID-19[35]. As COVID-19 switches from pandemic to endemic, it will be important to track how these recommendations evolve over time.
Patient-related barriers to appropriate surveillance of HCC were reportedly diverse and complex, creating additional obstacles to timely screening and early diagnosis of HCC in high-risk patients. Prior studies have identified similar barriers, including abdominal ultrasound lead time had an inverse relationship with surveillance; therefore, abdominal ultrasounds that were ordered further in advance were less likely to be completed. Furthermore, distance from the surveillance center has been identified as a notable factor, where patients with greater distance from the local hospital had lower rates of surveillance[37]. Another study in Dallas County evaluated patient-related characteristics regarding surveillance in cirrhotic patients. Factors associated with a higher level of overall knowledge and surveillance included Caucasian race, English as a primary language, HCV–related cirrhosis, Childs-Pugh A cirrhosis, receipt of hepatology subspecialty care, higher educational background, and higher perceived likelihood of dying from HCC[38]. A retrospective study in Dallas County evaluating HCC surveillance among cirrhotic patients in economically diverse cohorts revealed that inconsistent surveillance was associated with insurance status, African-American race, non-alcoholic steatohepatitis, and extrahepatic cancers[39]. Further highlighting the difference in socioeconomic status and its relationship with HCC screening, one study identified higher rates of HCC among Hispanics, African-Americans, and Asian Pacific Islanders compared to Caucasians. The foundation for these health disparities was perceived to be due to a combination of environmental, social, and economic variables, all factors that need to be addressed to advance health equity in HCC surveillance.
Consistently among studies, patient-level barriers to surveillance have included: transportation cost of surveillance studies, and scheduling conflicts, all of which were noted to contribute to poor HCC surveillance[38,40]. Many of these concerns were also voiced in our interviews with providers regarding patient-level barriers to appropriate surveillance. As the purpose of the surveillance guidelines is earlier initiation of intervention, reduction in overall morbidity and mortality, and reduction of financial burden on the healthcare system, patient-related barriers to screening are obstacles that may not be easily resolved[41]. One study reported that quality improvement measures with automatic surveillance reminders increased surveillance rates by 17%; while this would help eliminate scheduling concerns, it does not address issues with transportation[42]. Certainly, improvements may be made in order to accommodate patient-level barriers and address common concerns; however, providers must also address multi-variable patient -related barriers on an individual patient basis.
Health literacy refers to a patient’s ability to retrieve, comprehend, analyze, and apply medical information and contributes to low widespread cancer surveillance. Studies have remarked that health literacy impacts surveillance and treatment compliance of a variety of cancers, including breast, prostate, and cervical cancer. To highlight the impact of health literacy on surveillance in cirrhotic patients in particular, one study compared 6-month surveillance visits during an HCC pre-education phase and an HCC post-education phase with evidence of nearly 30% improvement in surveillance compliance in the post-education phase, after patients received educational exposure about HCC, across all literacy groups. Health literacy was an important barrier to HCC surveillance noted in this study.
Providers in our study suggested several interventions to improve HCC surveillance, including patient education, provider education, mass media campaigns, the use of technology tools, the introduction of patient navigators, improved collaboration between hepatology and primary care collaboration, and the involvement of radiology in recommending further surveillance studies. Several studies have evaluated retrospectively, or tested prospectively, interventions to improve HCC surveillance in high-risk patients. Commonly evaluated interventions targeted patients, providers, and the system. Patient-targeted interventions that have been previously tested include the use of outreach reminders to patients, improved patient education, and the use of outreach nurses[43-50]. Provider-targeted interventions included clinical reminders in the electronic medical record to remind providers to order HCC surveillance, inform them of overdue HCC surveillance, or to alert them to missed patient appointments, the use of provider compliance reports, and provider education[24,46,50-52]. System-level interventions included the utilization of novel web-based clinical tools to facilitate the identification of patients eligible for HCC surveillance, track these patients and their test results, and coordinate their follow-up care[42,53]. Opportunities to implement these previously tested interventions and those suggested by our study participants should be considered in designing future interventions, especially those that attempt to address provider-, system- and patient-level barriers such as those we have identified.
There are several important limitations to this study. First, the study was conducted at a large, urban, tertiary-care, and academic medical center with distinct specialization between general gastroenterologists and hepatologists and a robust internal referral system. Its generalizability to rural and community care settings may be limited. We believe that our findings regarding barriers to surveillance for HCC are robust, given the saturation in our data collection. However, providers from other institutions may have different perspectives based on their own experiences. Additionally, some of the recommendations suggested as opportunities to improve HCC surveillance will require further refinement and pilot testing. Finally, the scope of this study was limited to physician and nurse practitioner providers in primary care, gastroenterology, and hepatology. Other providers who care for similar patient populations may have alternative perspectives.
There are several important future directions for this work. First, patient perspectives should be examined using a combination of surveys, semi-structured interviews, and focus groups to elucidate the barriers most experienced by patients and what solutions they would find most efficacious. Second, the impact of social determinants of health, including safe housing, transportation, and neighborhoods; racism, discrimination, and violence; education, job opportunities and income; access to nutritious foods and physical activity; polluted air and water; and language and literacy skills, on HCC surveillance should be evaluated. Third, using a community-engaged approach involving patients as partners, considering local contexts, and including high-risk patients and HCC survivors, and building on work done to improve other types of cancer screening, interventions should be designed to address low rates of HCC surveillance. Finally, rigorous prospective comparative efficacy studies should be designed to test these proposed interventions in variable settings.
In conclusion, in this qualitative study of provider perspectives about HCC surveillance, several important themes were identified as we characterized provider-, system- and patient-level barriers to surveillance. When designing and implementing interventions to improve HCC surveillance among high-risk patients, it will be important to consider how to address these barriers so that both surveillance rates and health equity can be improved.
DECLARATIONS
Acknowledgments
The authors would like to acknowledge The Center for Advancement of Team Science, Analytics, and Systems Thinking in Health Services and Implementation Science Research (CATALYST), at the Ohio State University, for providing resources for this study including Atlas.ti subscriptions, access to transcription software and research assistant time for transcription and qualitative data coding and analysis.
Authors’ contributions
Study Design: Beal EW, Volney J, Sova L, McAlearney AS, Tsung A
Resources: McAlearney AS, Tsung A
Data Collection: Beal EW
Data Coding: Beal EW , Volney J, Sova L
Data Analysis: Beal EW, Gorji L, Volney J, Sova L, McAlearney AS, Tsung A
Data Interpretation: Beal EW, Gorji L, Volney J, Sova L, McAlearney AS, Tsung A
Manuscript Preparation: Beal EW, Gorji L
Manuscript Revision: Beal EW, Gorji L, Volney J, Sova L, McAlearney AS, Tsung A
Approval of Final Manuscript for Publication: Beal EW, Gorji L, Volney J, Sova L, McAlearney AS, Tsung A
Availability of data and materials
Data will be shared upon reasonable request to the corresponding author.
Financial support and sponsorship
Dr. Beal’s work was supported by a Pelotonia Postdoctoral Research Fellowship
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Approval was provided by the Institutional Review Board of the Ohio State University (2020C0163). All participants provided verbal informed consent prior to participation.
Consent for publication
All authors have reviewed the final version of the manuscript and provided consent for publication.
Copyright
© The Author(s) 2023.
REFERENCES
1. Akinyemiju T, Abera S, Ahmed M, et al; Global Burden of Disease Liver Cancer Collaboration. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the global burden of disease study 2015. JAMA Oncol 2017;3:1683-91.
2. Kanwal F, Singal AG. Surveillance for hepatocellular carcinoma: current best practice and future direction. Gastroenterology 2019;157:54-64.
3. Singal AG, Pillai A, Tiro J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med 2014;11:e1001624.
4. Yang B, Zhang B, Xu Y, et al. Prospective study of early detection for primary liver cancer. J Cancer Res Clin Oncol 1997;123:357-60.
5. Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol 2004;130:417-22.
6. Heimbach JK, Kulik LM, Finn RS, et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018;67:358-80.
7. Omata M, Cheng AL, Kokudo N, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int 2017;11:317-70.
8. Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018;69:182-236.
9. Covey AM. Hepatocellular carcinoma: updates to screening and diagnosis. J Natl Compr Canc Netw 2018;16:663-5.
10. Singal AG, Yopp A, S Skinner C, Packer M, Lee WM, Tiro JA. Utilization of hepatocellular carcinoma surveillance among American patients: a systematic review. J Gen Intern Med 2012;27:861-7.
11. Sloane D, Chen H, Howell C. Racial disparity in primary hepatocellular carcinoma : tumor stage at presentation, surgical treatment and survival. J Natl Med Assoc 2006;98:1934-9.
12. Ha J, Yan M, Aguilar M, et al. Race/ethnicity-specific disparities in cancer incidence, burden of disease, and overall survival among patients with hepatocellular carcinoma in the United States. Cancer 2016;122:2512-23.
13. Singal AG, Yopp AC, Gupta S, et al. Failure rates in the hepatocellular carcinoma surveillance process. Cancer Prev Res 2012;5:1124-30.
14. El-Serag HB, Alsarraj A, Richardson P, et al. Hepatocellular carcinoma screening practices in the department of veterans affairs: findings from a national facility survey. Dig Dis Sci 2013;58:3117-26.
15. Shavers VL, Brown ML. Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst 2002;94:334-57.
16. Parikh ND, Tayob N, Al-Jarrah T, et al. Barriers to surveillance for hepatocellular carcinoma in a multicenter cohort. JAMA Netw Open 2022;5:e2223504.
17. Beal EW, Owen M, McNamara M, McAlearney AS, Tsung A. Patient-, provider-, and system-level barriers to surveillance for hepatocellular carcinoma in high-risk patients in the USA: a scoping review. J Gastrointest Cancer 2023;54:332-56.
18. Simmons OL, Feng Y, Parikh ND, Singal AG. Primary care provider practice patterns and barriers to hepatocellular carcinoma surveillance. Clin Gastroenterol Hepatol 2019;17:766-73.
19. Dalton-Fitzgerald E, Tiro J, Kandunoori P, Halm EA, Yopp A, Singal AG. Practice patterns and attitudes of primary care providers and barriers to surveillance of hepatocellular carcinoma in patients with cirrhosis. Clin Gastroenterol Hepatol 2015;13:791-8.e1.
20. Glaser BG. More grounded theory methodology: a reader. Available from: https://www.amazon.com/More-Grounded-Theory-Methodology-reader/dp/188415607X[Last accessed on 25 Oct 2023].
21. Crabtree B, Miller W. Doing qualitative research. Available from: https://www.amazon.com/CRABTREE-QUALITATIVE-RESEARCH-Research-Paperback/dp/0761914986 [Last accessed on 25 Oct 2023].
22. Constas MA. Qualitative analysis as a public event: the documentation of category development procedures. Am Educ Res J 1992;29:253-66.
23. ATLAS.ti (Software). Available from: https://atlasti.com/ [Last accessed on 25 Oct 2023].
24. Beste LA, Ioannou GN, Yang Y, Chang MF, Ross D, Dominitz JA. Improved surveillance for hepatocellular carcinoma with a primary care-oriented clinical reminder. Clin Gastroenterol Hepatol 2015;13:172-9.
25. Russo MW, Fix OK, Koteish AA, et al. Modeling the hepatology workforce in the United States: a predicted critical shortage. Hepatology 2020;72:1444-54.
26. Russo MW, Koteish AA, Fuchs M, Reddy KG, Fix OK. Workforce in hepatology: update and a critical need for more information. Hepatology 2017;65:336-40.
27. Ladhani S, Ohri A, Wong RJ. Disparities in hepatocellular carcinoma surveillance: dissecting the roles of patient, provider, and health system factors. J Clin Gastroenterol 2020;54:218-26.
28. Toyoda H, Huang DQ, Le MH, Nguyen MH. Liver care and surveillance: the global impact of the COVID-19 pandemic. Hepatol Commun 2020;4:1751-7.
29. Mancebo G, Solé-Sedeño JM, Membrive I, et al. Gynecologic cancer surveillance in the era of SARS-CoV-2 (COVID-19). Int J Gynecol Cancer 2021;31:914-9.
30. D'Ovidio V, Lucidi C, Bruno G, Lisi D, Miglioresi L, Bazuro ME. Impact of COVID-19 pandemic on colorectal cancer screening program. Clin Colorectal Cancer 2021;20:e5-11.
31. Vose JM. Delay in cancer screening and diagnosis during the COVID-19 pandemic: what is the cost? Oncology 2020;34:343.
32. London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform 2020;4:657-65.
33. Zeng G, Gill US, Kennedy PTF. Prioritisation and the initiation of HCC surveillance in CHB patients: lessons to learn from the COVID-19 crisis. Gut 2020;69:1907-12.
34. Paredes AZ, Hyer JM, Beal EW, et al. Impact of skilled nursing facility quality on postoperative outcomes after pancreatic surgery. Surgery 2019;166:1-7.
35. Mehta N, Parikh ND, Kelley RK, Hameed B, Singal AG. Surveillance and monitoring of hepatocellular carcinoma during the COVID-19 pandemic. Clin Gastroenterol Hepatol 2021;19:1520-30.
36. Seo YS, Jang BK, Um SH, et al. Validation of risk prediction models for the development of HBV-related HCC: a retrospective multi-center 10-year follow-up cohort study. Oncotarget 2017;8:113213-24.
37. Goldberg DS, Taddei TH, Serper M, et al. Identifying barriers to hepatocellular carcinoma surveillance in a national sample of patients with cirrhosis. Hepatology 2017;65:864-74.
38. Farvardin S, Patel J, Khambaty M, et al. Patient-reported barriers are associated with lower hepatocellular carcinoma surveillance rates in patients with cirrhosis. Hepatology 2017;65:875-84.
39. Singal AG, Li X, Tiro J, et al. Racial, social, and clinical determinants of hepatocellular carcinoma surveillance. Am J Med 2015;128:90.e1-7.
40. Guo A, Pomenti S, Wattacheril J. Health disparities in screening, diagnosis, and treatment of hepatocellular carcinoma. Clin Liver Dis 2021;17:353-8.
41. Fitzmorris P, Singal AK. Surveillance and diagnosis of hepatocellular carcinoma. Gastro Hepat 2015;11:38-46.
42. Aberra FB, Essenmacher M, Fisher N, Volk ML. Quality improvement measures lead to higher surveillance rates for hepatocellular carcinoma in patients with cirrhosis. Dig Dis Sci 2013;58:1157-60.
43. Singal AG, Tiro JA, Marrero JA, et al. Mailed outreach program increases ultrasound screening of patients with cirrhosis for hepatocellular carcinoma. Gastroenterology 2017;152:608-15.e4.
44. Singal AG, Tiro JA, Murphy CC, et al. Mailed outreach invitations significantly improve HCC surveillance rates in patients with cirrhosis: a randomized clinical trial. Hepatology 2019;69:121-30.
45. Yoder L, Mladenovic A, Pike F, et al. Attendance at a transitional liver clinic may be associated with reduced readmissions for patients with liver disease. Am J Med 2022;135:235-43.e2.
46. Kennedy NA, Rodgers A, Altus R, McCormick R, Wundke R, Wigg AJ. Optimisation of hepatocellular carcinoma surveillance in patients with viral hepatitis: a quality improvement study. Intern Med J 2013;43:772-7.
47. Shaw J, Patidar KR, Reuter B, et al. Focused education increases hepatocellular cancer screening in patients with cirrhosis regardless of functional health literacy. Dig Dis Sci 2021;66:2603-9.
48. Artinyan A, Mailey B, Sanchez-Luege N, et al. Race, ethnicity, and socioeconomic status influence the survival of patients with hepatocellular carcinoma in the United States. Cancer 2010;116:1367-77.
49. Nam JY, Lee JH, Kim HY, et al. Oral medications enhance adherence to surveillance for hepatocellular carcinoma and survival in chronic hepatitis B patients. PLoS One 2017;12:e0166188.
50. Cabrie T, Wheeler E, Jacqui R, et al. The challenge of liver cancer surveillance in general practice: Do recall and reminder systems hold the answer? Available from: https://www.racgp.org.au/afp/2017/november/the-challenge-of-liver-cancer-surveillance/ [Last accessed on 27 Oct 2023].
51. Cahill JA, Rizvi S, Saeian K. Assessment of adherence to baseline quality measures for cirrhosis and the impact of performance feedback in a regional VA medical center. Am J Med Qual 2018;33:262-8.
52. Rogal SS, Yakovchenko V, Gonzalez R, et al. The hepatic innovation team collaborative: a successful population-based approach to hepatocellular carcinoma surveillance. Cancers 2021;13:2251.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Beal EW, Gorji L, Volney J, Sova L, McAlearney AS, Tsung A. Barriers to surveillance for hepatocellular cancer among patients with chronic liver disease -providers' perspectives. Hepatoma Res 2023;9:45. http://dx.doi.org/10.20517/2394-5079.2023.75
AMA Style
Beal EW, Gorji L, Volney J, Sova L, McAlearney AS, Tsung A. Barriers to surveillance for hepatocellular cancer among patients with chronic liver disease -providers' perspectives. Hepatoma Research. 2023; 9: 45. http://dx.doi.org/10.20517/2394-5079.2023.75
Chicago/Turabian Style
Beal, Eliza W., Leva Gorji, Jaclyn Volney, Lindsey Sova, Ann Scheck McAlearney, Allan Tsung. 2023. "Barriers to surveillance for hepatocellular cancer among patients with chronic liver disease -providers' perspectives" Hepatoma Research. 9: 45. http://dx.doi.org/10.20517/2394-5079.2023.75
ACS Style
Beal, EW.; Gorji L.; Volney J.; Sova L.; McAlearney AS.; Tsung A. Barriers to surveillance for hepatocellular cancer among patients with chronic liver disease -providers' perspectives. Hepatoma. Res. 2023, 9, 45. http://dx.doi.org/10.20517/2394-5079.2023.75
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 4 clicks
Cite This Article 4 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.