Hepatocellular carcinoma on the background of nonalcoholic fatty liver disease: epidemiological update
Abstract
The epidemiological features of hepatocellular carcinoma have changed significantly in the last decades. While for a long-time viral hepatitis and alcohol consumption have been the leading risk factors, the current spread of obesity and type 2 diabetes has contributed to the emergence of non-alcoholic fatty liver disease (NAFLD) worldwide, which has become the leading chronic liver disease as well as one of the main etiologies of hepatocellular carcinoma (HCC), especially in western countries. In this review, we resume the latest data about the epidemiology of metabolic liver disease and HCC arising from NAFLD and discuss the main clinical and molecular features leading to the progression of liver disease and the development of HCC in NAFLD. The emerging concept of metabolic associated fatty liver disease and its association with the development of HCC are also introduced.
Keywords
INTRODUCTION
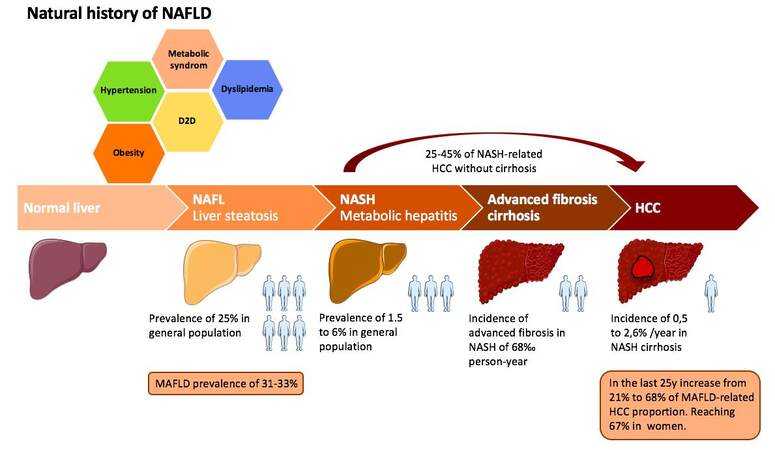
Non-alcoholic fatty liver disease (NAFLD) is today one of the main chronic liver diseases and a leading cause of hepatocellular carcinoma (HCC) worldwide[1]. Its emergence over the past decades, parallel to the decrease in the prevalence of hepatitis C, is partly explained by the global increase in obesity and type 2 diabetes (T2D) since the end of the 20th century[2,3]. Surgical series suggest that 25-45% of HCCs develop in a non-cirrhotic liver during NAFLD[4,5]. In this review, we summarize the latest data on the epidemiology of NAFLD-related HCC and discuss its genetic, epigenetic, and pathogenic mechanisms.
DEFINITION AND EPIDEMIOLOGY OF NAFLD WORLDWIDE
NAFLD is commonly defined as the continuum of two distinct pathological entities [Figure 1], associated with different progression and severity profiles[6,7]. Non-alcoholic fatty liver, considered to be a slow and non-aggressive condition with a low risk of progressing to severe liver disease[8,9], is characterized by the presence of histological steatosis in more than 5% of hepatocytes, without hepatocellular injury and steatohepatitis, and is rarely associated with transaminase disturbances. Non-alcoholic steatohepatitis (NASH), defined by steatosis (> 5%) associated with lobular inflammation and hepatocyte ballooning with or without fibrosis, is considered to be a more aggressive condition. Metabolic factors are associated with progression to NAFLD: dyslipidemia (69%), obesity (51%), metabolic syndrome (43%), arterial hypertension (39%),and T2D (22%)[1].
Alcoholic liver disease (ALD) shares with NAFLD and NASH some common histological features, including steatosis, inflammation, hepatocellular ballooning, and Mallory bodies, but NAFLD is an exclusion diagnosis, traditionally defined in opposition to ALD[10,11]. The diagnosis of NAFLD can therefore be made after excluding excessive alcohol consumption and eliminating the other risk factors for chronic liver disease and the secondary causes of steatosis such as drugs, toxic substances, or undernutrition. A recent international expert consensus statement proposes another definition of the liver disease linked to metabolic syndrome[12]. Thus, the term metabolic associated fatty liver disease (MAFLD) meets positive diagnostic criteria for liver disease associated with a metabolic disorder, independently of other causes of liver disease. Given the major increase in its prevalence in the world, this nomenclature considers MAFLD as an autonomous disease, not excluding the coexistence of other chronic liver diseases, in particular ALD. The diagnostic criteria of MAFLD are based on the demonstration of hepatic steatosis by histology, imaging, or non-invasive tools, associated with at least one criterion among obesity/overweight, T2D, or a normal weight with the presence of at least two metabolic disorders (pre-diabetes, HDL hypocholesterolemia, hypertriglyceridemia, augmented waist circumference, hypertension, augmentation of plasma high-sensitivity C-reactive protein level, and positive HOMA score). In clinical practice, patients with MAFLD frequently present cofactors of chronic liver disease. Indeed, the association of MAFLD with excessive alcohol consumption is frequent, estimated at 46% of patients with NAFLD-related HCC in an Italian multicenter cohort[13], and some studies suggest that moderate alcohol consumption may slow the regression of steatosis and NASH and worsen the progression of liver fibrosis[14,15].
NAFLD is one of the leading chronic liver diseases in the world today, its overall prevalence being estimated at nearly 25% in the general population[1,16,17]. The emergence of NAFLD over the past decade may be explained in part by the global increase in the prevalence of obesity and T2D since the end of the 20th century[3,18,19]. Despite the global rise in its incidence and prevalence, the distribution of metabolic liver disease is heterogeneous around the world with the highest prevalence reported in the Middle East (32%) and South America (31%) and the lowest distribution in Africa (14%)[1]. The epidemiology of NAFLD in Europe and the United States is relatively similar, with a very heterogeneous prevalence varying from 4% to 50% depending on the country in Europe and from 11% to 46% depending on the study in the United States[1,20]. The analysis of the French CONSTANCES cohort permitted estimating the prevalence of NAFLD at 18.2% of the general population[21], reaching 80% in obese patients and 60% in diabetic patients; the risk of NAFLD also increased with age. Moreover, in the United States, NAFLD is nowadays the primary etiology of cirrhosis in some cohorts[22,23]. In Asia, the emergence of NAFLD could be associated with changes in economic, ethnic, and lifestyle conditions, with a prevalence varying from 15% to 44% depending on the country, being higher in Southeast Asia, suggesting that NAFLD is no longer a “western disease”[1,24,25].
The overall prevalence of NASH in the general population is currently estimated between 1.5% and 6.5% worldwide. In France, national data suggest an overall prevalence of 2.6%. In the United States, NASH appears to be the second indication for liver transplantation (LT) behind ALD[1,9,16,22]. Epidemiological modeling estimates a 21% increase in the prevalence of NAFLD between 2015 and 2030 and a 63% increase in the prevalence of NASH during the same period[26].
NAFLD NATURAL HISTORY: FROM STEATOSIS TO HCC
According to some prospective studies based on paired biopsies, NAFL may progress to NASH[27,28], implying an increased risk of progression to liver damage and liver-related death. The risk of progression from NAFL to NASH is estimated at around 15–20%[1,9](Figure 1). The mean progression of hepatic fibrosis in NASH patients is less than 0.1%, with an estimated incidence of severe fibrosis of 68 per 1000 person-years[8]. In the French CONSTANCES cohort, the prevalence of advanced fibrosis was 7.6% in NAFLD patients with T2D[21].
NASH is associated with an increased death rate compared to the general population, and cardiovascular disease is believed to be the leading cause of death in these patients[29]. However, some recent data suggest that the risk of complications and mortality in NASH is also related to the severity of liver fibrosis[30-32]. In fact, in a Swedish histopathological study conducted in a cohort between 1966 and 2017, the absolute risk of death at 20 years progressively increased by 11% in NAFL, 18.5% in NASH without fibrosis, and 49% in NASH-induced cirrhosis, compared to the general population; however, this excess mortality was mainly due to extrahepatic cancers and cirrhosis[33]. In the American prospective cohort of Sanyal et al.[31], NAFLD patients with stage F4 fibrosis had higher all-cause and liver-related mortality compared to fibrosis stages F0 to F2 (HRs of 3.9 and 12.7, respectively). HCC is also an independent risk factor for liver-related mortality in patients with NASH. In fact, in two prospective studies conducted in the United States and Japan, HCC was the cause of 45% of deaths in patients with NASH[34,35].
During the 1980s, the main risk factors for HCC were related to viral hepatitis and alcohol. The recent decrease in the prevalence of hepatitis C thanks to the advent of direct-acting antiviral treatments and reduction of transmission and the better control of hepatitis B has changed the etiological profile of HCC worldwide[2,36,37]. NASH is currently one of the main causes of HCC in the world: in the 2000s, it was responsible for 14% and 34% of HCCs in the United States and England, respectively, and today represents the second etiology of HCC treated with LT in the United States[38,39]. However, the incidence data for NAFLD-related HCC currently available are very heterogeneous, varying from 0.25% to 7.6% depending on the population study[40][Figure 1].
The presence of NASH, advanced liver fibrosis, and cirrhosis are recognized risk factors for progression to HCC[32,41]. According to a recent meta-analysis, the incidence of HCC in patients with NAFL was 0.44 per 1000 person-years, and it as 5.29 per 1000 person-years in NASH, which is still lower than the incidence found in other chronic diseases of the liver, especially viral liver disease[1]. As observed in other chronic liver diseases, the HCC developed on NASH occurs mainly in the context of advanced fibrosis[29,31,32,41,42]. Nevertheless, surgical series suggest that 25-45% of HCCs develop in the absence of cirrhosis in NASH. Male sex is a major risk factor for developing NASH-related HCC in the absence of cirrhosis[4,5,13,16,43]. A recent meta-analysis reported that, in patients with NASH-related HCC, the likelihood of not having cirrhosis was five times that of patients with HCC related to chronic hepatitis C, with a prevalence of cirrhosis of 35% in NASH-related HCC, against 9% in hepatitis C, 8% in hepatitis B, and 11% in ALD[4,8]. Compared with other etiologies of chronic liver disease, patients developing HCC on NASH appear to be older, and several studies suggest a less favorable oncological prognosis, with tumors diagnosed at a more advanced stage and shorter survival[44-46].
Since the proposal of an alternative nomenclature (MAFLD), few studies have explored the impact of this condition on the development of HCC. A Swiss study analyzing regional data on HCC over a 25-year period found an increase in the incidence of HCC associated with MAFLD between 1990 and 2014, particularly in women, with an increase from 21% to 68% between the periods 1990-1994 and 2010-2014, respectively, along with the increase in the prevalence of obesity from 26% to 41%[47]. In another study conducted in the United States using the NHANES III database comparing the characteristics of MAFLD (31% of participants) and NAFLD (33% of participants) patients, MAFLD patients were significantly older and had a higher proportion of metabolic comorbidities and altered liver enzymes. The authors concluded that the MAFLD nomenclature was more effective in identifying patients at risk for fibrosis progression[48].
Although there is still a lack of reliable data to assess the prevalence of HCC associated with NAFLD, some estimates have been made in predictive models. Unlike the predicted decline in HBV- and HCV-related HCC in many parts of the world, NAFLD-related HCC is expected to increase. A Markov model built on the basis of expected future frequencies of metabolic factors in the United States[26] estimated that the HCC prevalence will increase by 63% in NASH patients and 146% in NAFLD patients by 2030. Considering the progression of metabolic factors in the population, the authors calculated that, in 2030, 72% of the annual incidence of HCC will occur in patients with NASH-induced cirrhosis, compared to 64% in 2015. Another predictive epidemiological model at the international level estimated 86% and 125% growths in cases of HCC linked to NAFLD between 2016 and 2030 in China and France, respectively[49].
MOLECULAR PATTERNS INVOLVED IN NAFLD INITIATION AND PROGRESSION
Certain hereditary factors as well as ethnicity could affect the susceptibility to the development and progression of NAFLD. In patients of Hispanic origin, for example, the proportion of NAFL and NASH in patients with hepatic metabolic disease is high, while a lower rate is reported in people of non-Hispanic African American origin[50,51]. The difference in the distribution of NAFLD based on ethnic variations has in particular been attributed to the polymorphism of PNPLA3 (encoding the protein 3 containing the domain of the patatin-type phospholipase or adiponutrin)[52-54]. Furthermore the presence of polymorphism rs738409 C > G in PNPLA3 has been linked to hepatic triglyceride accumulation[42,52,55] and associated with an higher risk of fibrosis progression and development of NASH-related HCC[41,56-58]. Other single nucleotide polymorphisms have been described in NAFDL, notably the rs58542926 C > T variant of TM6SF2 (transmembrane 6 superfamily member 2) linked to development of NAFLD, progression to cirrhosis, and HCC development in ALD and NAFLD[59-62]. The rs641738 C > T polymorphism of the gene encoding membrane-bound O-acyltransferase domain containing 7 (MBOAT7) promotes hepatocellular triglyceride accumulation and production of inflammatory mediators and is associated with an increased risk of progression to NAFLD, progression of hepatic fibrosis, and of HCC development during NAFLD[62-64]. Moreover, the rs72613567 polymorphism of the 17β-hydroxysteroid dehydrogenase 13 gene (HSD17B13) seems to have a protective effect on the progression of histological parameters in NASH, in particular on lobular inflammation, hepatocellular ballooning, and fibrosis[62,63,65].
Pinyol et al.[66] recently described the mutational landscape of HCC linked to NASH and identified as main mutations the promoter TERT (56%), CTNNB1 (28%), TP53 (18%), and ACVR2A (10%), with a higher rate of ACVR2A mutations and a lower rate of TP53 mutations in NASH-related HCC compared to HCC related to other etiologies.
Furthermore, a recent genome-wide DNA methylation analysis identified alterations in DNA methylation that are specific to NASH liver tissue and NASH-related HCC and not detected in samples of patients with virus related-HCC (e.g., dysregulation of MAML3 and WHSC1 genes methylation), suggesting that this modification could participate in hepatocarcinogenesis[67]. Among epigenetic alterations, a reduction of global and gene-specific histone H4K16 acetylation has also been reported in NASH-related hepatocarcinogenesis in mice, which induces silencing of genes related to cell death[68]. Several studies have described dysregulation of non-coding microRNA (miRNA) during the development of NASH and the transition to HCC, in particular downregulation of microRNA-122 and upregulation of microRNA -34a[69].
Currently, many studies are looking for clinical applications of these molecular deregulations for the risk stratification of HCC in NAFLD. Notably, a genetic risk score was elaborated by Gellert-Kristensen et al.[70] based on the sum of three risk-increasing alleles (PNPLA3, TM6SF2, and HSD17B13) to predict the risk of progression to cirrhosis and HCC development in NAFLD. Another genetic risk score has been proposed based on several variants (PNPLA3, TM6SF2, GCKR, and MBOAT7) to assess the risk of HCC development in NAFLD patients without severe liver fibrosis or obesity[71]. However, further studies are needed to validate the use and feasibility of these genetic scores in clinical practice.
Alteration of the gut–liver axis appears to play an essential role in liver damage and progression of liver disease[72]. Chronic liver disease and cirrhosis are associated with low gut microbial diversity and increased gut permeability compared to healthy patients[73-75]; the liver is more exposed to pathogen-associated molecular patterns and bacterial metabolites causing a persistent inflammation[74]. Furthermore, obesity, T2D, and metabolic syndrome are associated with a dysbiotic intestinal microbiota, in particular with an increase in the Firmicutes/Bacteroidetes ratio and a decrease in microbiota diversity[74,76]. In NASH, increased gut permeability results in endotoxemia, which has been shown to trigger inflammatory cytokine responses and insulin resistance[72]. In humans, plasma levels of IgG against endotoxin appear to be higher in NASH; moreover, the levels gradually increase with NASH grade, suggesting a relationship between chronic exposure and the severity of histological findings[77,78]. The alteration of the gut microbiota in NAFLD also affects bile acid metabolism, decreasing the biotransformation of primary bile acids, thereby altering intestinal permeability and promoting bacterial translocation, which contribute to liver damage[74,79]. Additionally, the increase in endogenous ethanol produced by the microbiota in NASH patients may contribute to the development of fibrosis and progression to cirrhosis by activating liver stellate cells[74]. In mice models, the degree of steatosis and lobular inflammation were enhanced by a high-fat diet and impaired integrity of the intestinal barrier, suggesting a central role of bacterial translocation in the progression of NAFLD[72]. The link between the gut microbiota and hepatocarcinogenesis has also been studied in NAFLD. A recent study in humans suggests that NAFLD cirrhotic patients with HCC had increased intestinal inflammation and expression of pro-inflammatory cytokines and chemokines compared to those without HCC or healthy subjects[80]. A high-cholesterol diet led to progression to steatohepatitis, fibrosis, and the development of HCC in mice, with a gradually altered gut microbiota[81,82]. However, to date, the contribution of NASH-associated dysbiosis in the development of HCC is mainly based on animal models.
NAFLD DIAGNOSIS, SURVEILLANCE, AND HCC SCREENING
The gold standard for the diagnosis of NAFL and NASH remains hepatic biopsy. However, several non-invasive tools have been developed to quantify the steatosis: CAP, attenuation of sound signals measured by impulse elastometry; FLI, predictive score for steatosis calculated from clinical and biological parameters; and SteatoTest®, NAFLD Liver Fat Score. Other non-invasive tools are accessible for the evaluation of fibrosis stage (elastometry, Fib4, NAFLD Fibrosis Score, Fibrotest®, FibroMetre®, and ELF™); however, to date, there are no tools capable of correctly assessing the degree of inflammation and thus discriminating between NASH and NAFL[83]. Screening for NAFLD, by ultrasound (and/or steatosis biomarkers) and liver enzyme dosage, is currently recommended by EASL in patients with metabolic syndrome, obesity, T2D, or elevated liver enzymes in the presence of metabolic risk factors[29]. However, these recommendations do not achieve consensus around the world. In the United States, for example, the AASLD does not recommend screening for NAFLD, including in high-risk groups, given the lack of evidence of cost-effectiveness[9], while, in Asia, the Asian Pacific Association for the Study of the Liver proposes considering screening in obese or diabetic patients[84].
Liver ultrasound is the gold standard for HCC screening in patients with NASH cirrhosis[9,29]; however, the presence of liver steatosis and obesity can make it difficult to visualize deep structures on ultrasound[85,86]. Indeed, in a retrospective analysis of ultrasound data in a cohort of 941 patients with cirrhosis in the United States[86], obesity and NASH were factors associated in multivariate analysis with insufficient quality of the ultrasound examination. In this context, Park et al.[87] evaluated in a prospective cohort the performance of unenhanced MRI for the detection of HCC in patients with cirrhosis at high risk for HCC. Unenhanced T2-weighted or diffusion-weighted MRI had a sensitivity of 79% and a negative predictive value of 99% for the detection of HCC in the context of screening, compared with 28% and 97%, respectively, with ultrasound (P < 0.001). More data are needed to assess the contribution and feasibility of MRI in screening for HCC in NASH cirrhosis in clinical practice.
In the 2016 cohort of Piscaglia et al.[13], only 48% of NAFLD-related HCCs were diagnosed as part of a screening program, compared to 63% for HCCs associated with HCV. Thus, a significant number of NASH-related cirrhosis would already be complicated by HCC at diagnosis, with hepatic tumors detected at a more advanced stage, limiting the access of these patients to curative treatment. The recommendations of the American Gastroenterological Association (AGA) propose initiating screening at the stage of F3 fibrosis (advanced fibrosis) in NAFLD patients[85]. However, given the large number of NAFLD patients at risk of developing HCC, it is currently not recommended in Europe to systematically screen for HCC in patients without cirrhosis[29,40]. Moreover, considering that about a third of HCCs develop in a non-cirrhotic liver during NAFLD and the absence of recommendation for screening in these patients at present, the diagnosis would be later and their prognosis altered[29]. In a prospective study by Tobari et al.[43], NAFLD-related HCCs without cirrhosis were larger compared to cirrhotic patients, and this difference was attributed to the lack of screening in these patients.
CONCLUSION
It is clear that the growing epidemics of NAFLD will dramatically influence the incidence of HCC. This perspective will lead to facing challenges of different nature. On one hand, we will be obliged to design new screening programs including a very large proportion of the population and thus requiring a sustained economic effort. On the other hand, the higher impact of co-morbidities and age of patients with NASH-related HCC will challenge us to offer a better tailored therapy. Furthermore, the efforts to simplify the nomenclatures with the proposition of MAFLD will introduce an additional variable to analyze. Few data are now available about the risk of developing HCC from MAFLD, and thus more data are needed to evaluate the necessity of a screening program in this setting.
DECLARATIONS
Authors’ contributionsParticipated in all stages of manuscript production, design, figures, writing and review of final versio: Desjonqueres E, Gigante E
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73-84.
2. Arora SS, Axley P, Ahmed Z, et al. Decreasing frequency and improved outcomes of hepatitis C-related liver transplantation in the era of direct-acting antivirals - a retrospective cohort study. Transpl Int 2019;32:854-64.
3. Younossi ZM, Stepanova M, Younossi Y, et al. Epidemiology of chronic liver diseases in the USA in the past three decades. Gut 2020;69:564-8.
4. Mittal S, El-Serag HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 2016;14:124-31.e1.
5. Yasui K, Hashimoto E, Komorizono Y, et al. Japan NASH Study Group; Ministry of Health; Labour; and Welfare of Japan. Characteristics of patients with nonalcoholic steatohepatitis who develop hepatocellular carcinoma. Clin Gastroenterol Hepatol 2011;9:428-33; quiz e50.
6. Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol 2015;13:643-54.e1.
7. Pais R, Charlotte F, Fedchuk L, et al. LIDO Study Group. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol 2013;59:550-6.
9. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology 2018;67:328-57.
10. Brunt EM, Wong VW, Nobili V, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primers 2015;1:15080.
11. Spech HJ, Liehr H, Mitschke H. [Nonalcoholic fatty liver hepatitis and fatty cirrhosis mimicking alcoholic liver diseases]. Z Gastroenterol 1983;21:651-9.
12. Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol 2020;73:202-9.
13. Piscaglia F, Svegliati-Baroni G, Barchetti A, et al. HCC-NAFLD Italian Study Group. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: a multicenter prospective study. Hepatology 2016;63:827-38.
14. Ajmera V, Belt P, Wilson LA, et al. Nonalcoholic Steatohepatitis Clinical Research Network. Among patients with nonalcoholic fatty liver disease, modest alcohol use is associated with less improvement in histologic steatosis and steatohepatitis. Clin Gastroenterol Hepatol 2018;16:1511-20.e5.
15. Chang Y, Cho YK, Kim Y, et al. Nonheavy drinking and worsening of noninvasive fibrosis markers in nonalcoholic fatty liver disease: a cohort study. Hepatology 2019;69:64-75.
16. Younossi ZM, Henry L. Epidemiology of non-alcoholic fatty liver disease and hepatocellular carcinoma. JHEP Rep 2021;3:100305.
17. Cotter TG, Rinella M. Nonalcoholic fatty liver disease 2020: the state of the disease. Gastroenterology 2020;158:1851-64.
19. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes - global burden of disease and forecasted trends. J Epidemiol Glob Health 2020;10:107-11.
20. Perumpail BJ, Khan MA, Yoo ER, Cholankeril G, Kim D, Ahmed A. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J Gastroenterol 2017;23:8263-76.
21. Nabi O, Lacombe K, Boursier J, Mathurin P, Zins M, Serfaty L. prevalence and risk factors of nonalcoholic fatty liver disease and advanced fibrosis in general population: the French nationwide NASH-CO study. Gastroenterology 2020;159:791-3.e2.
22. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology 2015;148:547-55.
23. Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology 2016;64:1969-77.
24. Farrell GC, Wong VW, Chitturi S. NAFLD in Asia--as common and important as in the West. Nat Rev Gastroenterol Hepatol 2013;10:307-18.
25. Li J, Zou B, Yeo YH, et al. Prevalence, incidence, and outcome of non-alcoholic fatty liver disease in Asia, 1999–2019: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2019;4:389-98.
26. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 2018;67:123-33.
27. Wong VW, Wong GL, Choi PC, et al. Disease progression of non-alcoholic fatty liver disease: a prospective study with paired liver biopsies at 3 years. Gut 2010;59:969-74.
28. McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol 2015;62:1148-55.
29. Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388-402.
30. Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology 2015;149:389-97.e10.
31. Sanyal AJ, Van Natta ML, Clark J, et al. NASH Clinical Research Network (CRN). Prospective study of outcomes in adults with nonalcoholic fatty liver disease. N Engl J Med 2021;385:1559-69.
32. Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, et al. fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology 2018;155:443-57.e17.
33. Simon TG, Roelstraete B, Khalili H, Hagström H, Ludvigsson JF. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: results from a nationwide cohort. Gut 2021;70:1375-82.
34. Yatsuji S, Hashimoto E, Tobari M, Taniai M, Tokushige K, Shiratori K. Clinical features and outcomes of cirrhosis due to non-alcoholic steatohepatitis compared with cirrhosis caused by chronic hepatitis C. J Gastroenterol Hepatol 2009;24:248-54.
35. Sanyal AJ, Banas C, Sargeant C, et al. Similarities and differences in outcomes of cirrhosis due to nonalcoholic steatohepatitis and hepatitis C. Hepatology 2006;43:682-9.
36. Valery PC, Laversanne M, Clark PJ, Petrick JL, McGlynn KA, Bray F. Projections of primary liver cancer to 2030 in 30 countries worldwide. Hepatology 2018;67:600-11.
37. Global hepatitis report, 2017 n.d. https://www.who.int/publications-detail-redirect/global-hepatitis-report-2017 [Last accessed on Mar 15, 2022].
38. Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology 2014;59:2188-95.
39. Dyson J, Jaques B, Chattopadyhay D, et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol 2014;60:110-7.
40. Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu., European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2018;69:182-236.
41. Anstee QM, Reeves HL, Kotsiliti E, Govaere O, Heikenwalder M. From NASH to HCC: current concepts and future challenges. Nat Rev Gastroenterol Hepatol 2019;16:411-28.
42. Allaire M, Dupont B, Nahon P, Ganne-carrié N, Nault JC. Hepatocellular carcinoma: the Impact of NAFLD. Curr Hepatology Rep 2016;15:190-8.
43. Tobari M, Hashimoto E, Taniai M, et al. The characteristics and risk factors of hepatocellular carcinoma in nonalcoholic fatty liver disease without cirrhosis. J Gastroenterol Hepatol 2020;35:862-9.
44. Younossi ZM, Otgonsuren M, Henry L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology 2015;62:1723-30.
45. Than NN, Ghazanfar A, Hodson J, et al. Comparing clinical presentations, treatments and outcomes of hepatocellular carcinoma due to hepatitis C and non-alcoholic fatty liver disease. QJM 2017;110:73-81.
46. Golabi P, Rhea L, Henry L, Younossi ZM. Hepatocellular carcinoma and non-alcoholic fatty liver disease. Hepatol Int 2019;13:688-94.
47. Myers S, Neyroud-Caspar I, Spahr L, et al. NAFLD and MAFLD as emerging causes of HCC: A populational study. JHEP Rep 2021;3:100231.
48. Lin S, Huang J, Wang M, et al. Comparison of MAFLD and NAFLD diagnostic criteria in real world. Liver Int 2020;40:2082-9.
49. Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol 2018;69:896-904.
50. Eslam M, Valenti L, Romeo S. Genetics and epigenetics of NAFLD and NASH: clinical impact. J Hepatol 2018;68:268-79.
51. Browning MG, Khoraki J, DeAntonio JH, et al. Protective effect of black relative to white race against non-alcoholic fatty liver disease in patients with severe obesity, independent of type 2 diabetes. Int J Obes (Lond) 2018;42:926-9.
52. Romeo S, Kozlitina J, Xing C, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 2008;40:1461-5.
53. Pan JJ, Fallon MB. Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol 2014;6:274-83.
54. Dongiovanni P, Anstee QM, Valenti L. Genetic predisposition in NAFLD and NASH: impact on severity of liver disease and response to treatment. Curr Pharm Des 2013;19:5219-38.
55. BasuRay S, Wang Y, Smagris E, Cohen JC, Hobbs HH. Accumulation of PNPLA3 on lipid droplets is the basis of associated hepatic steatosis. Proc Natl Acad Sci U S A 2019;116:9521-6.
56. Falleti E, Fabris C, Cmet S, et al. PNPLA3 rs738409C/G polymorphism in cirrhosis: relationship with the aetiology of liver disease and hepatocellular carcinoma occurrence. Liver Int 2011;31:1137-43.
57. Liu YL, Patman GL, Leathart JB, et al. Carriage of the PNPLA3 rs738409 C > G polymorphism confers an increased risk of non-alcoholic fatty liver disease associated hepatocellular carcinoma. J Hepatol 2014;61:75-81.
58. Seko Y, Sumida Y, Tanaka S, et al. Development of hepatocellular carcinoma in Japanese patients with biopsy-proven non-alcoholic fatty liver disease: Association between PNPLA3 genotype and hepatocarcinogenesis/fibrosis progression. Hepatol Res 2017;47:1083-92.
59. Kozlitina J, Smagris E, Stender S, et al. Exome-wide association study identifies a TM6SF2 variant that confers susceptibility to nonalcoholic fatty liver disease. Nat Genet 2014;46:352-6.
60. Liu YL, Reeves HL, Burt AD, et al. TM6SF2 rs58542926 influences hepatic fibrosis progression in patients with non-alcoholic fatty liver disease. Nat Commun 2014;5:4309.
61. Yang J, Trépo E, Nahon P, et al. PNPLA3 and TM6SF2 variants as risk factors of hepatocellular carcinoma across various etiologies and severity of underlying liver diseases. Int J Cancer 2019;144:533-44.
62. Nahon P, Allaire M, Nault JC, Paradis V. Characterizing the mechanism behind the progression of NAFLD to hepatocellular carcinoma. Hepat Oncol 2020;7:HEP36.
63. Campani C, Nault J. Molecular mechanisms of liver carcinogenesis related to metabolic syndrome. HR 2022; doi: 10.20517/2394-5079.2021.126.
64. Tanaka Y, Shimanaka Y, Caddeo A, et al. LPIAT1/MBOAT7 depletion increases triglyceride synthesis fueled by high phosphatidylinositol turnover. Gut 2021;70:180-93.
65. Motomura T, Amirneni S, Diaz-Aragon R, et al. Is HSD17B13 genetic variant a protector for liver dysfunction? J Pers Med 2021;11:619.
66. Pinyol R, Torrecilla S, Wang H, et al. Molecular characterisation of hepatocellular carcinoma in patients with non-alcoholic steatohepatitis. J Hepatol 2021;75:865-78.
67. Kuramoto J, Arai E, Tian Y, et al. Genome-wide DNA methylation analysis during non-alcoholic steatohepatitis-related multistage hepatocarcinogenesis: comparison with hepatitis virus-related carcinogenesis. Carcinogenesis 2017;38:261-70.
68. de Conti A, Dreval K, Tryndyak V, et al. Inhibition of the cell death pathway in Nonalcoholic Steatohepatitis (NASH)-related hepatocarcinogenesis is associated with histone H4 lysine 16 deacetylation. Mol Cancer Res 2017;15:1163-72.
69. Wong CM, Tsang FH, Ng IO. Non-coding RNAs in hepatocellular carcinoma: molecular functions and pathological implications. Nat Rev Gastroenterol Hepatol 2018;15:137-51.
70. Gellert-Kristensen H, Richardson TG, Davey Smith G, Nordestgaard BG, Tybjaerg-Hansen A, Stender S. Combined effect of PNPLA3, TM6SF2, and HSD17B13 variants on risk of cirrhosis and hepatocellular carcinoma in the general population. Hepatology 2020;72:845-56.
71. Bianco C, Jamialahmadi O, Pelusi S, et al. Non-invasive stratification of hepatocellular carcinoma risk in non-alcoholic fatty liver using polygenic risk scores. J Hepatol 2021;74:775-82.
72. Poeta M, Pierri L, Vajro P. Gut-liver axis derangement in non-alcoholic fatty Liver disease. Children (Basel) 2017;4:66.
73. Qin N, Yang F, Li A, et al. Alterations of the human gut microbiome in liver cirrhosis. Nature 2014;513:59-64.
74. Milosevic I, Vujovic A, Barac A, et al. Gut-Liver Axis, Gut Microbiota, and Its Modulation in the Management of Liver Diseases: A Review of the Literature. Int J Mol Sci 2019;20:395.
75. Tripathi A, Debelius J, Brenner DA, et al. The gut-liver axis and the intersection with the microbiome. Nat Rev Gastroenterol Hepatol 2018;15:397-411.
76. Dong TS, Luu K, Lagishetty V, et al. Gut microbiome profiles associated with steatosis severity in metabolic associated fatty liver disease. HR 2021; doi: 10.20517/2394-5079.2021.55.
77. Cani PD, Amar J, Iglesias MA, et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 2007;56:1761-72.
78. Verdam FJ, Rensen SS, Driessen A, Greve JW, Buurman WA. Novel evidence for chronic exposure to endotoxin in human nonalcoholic steatohepatitis. J Clin Gastroenterol 2011;45:149-52.
79. Sinal CJ, Tohkin M, Miyata M, Ward JM, Lambert G, Gonzalez FJ. Targeted disruption of the nuclear receptor fxr/bar impairs bile acid and lipid homeostasis. Cell 2000;102:731-44.
80. Ponziani FR, Bhoori S, Castelli C, et al. Hepatocellular carcinoma is associated with gut microbiota profile and inflammation in nonalcoholic fatty liver disease. Hepatology 2019;69:107-20.
81. Schwabe RF, Greten TF. Gut microbiome in HCC - mechanisms, diagnosis and therapy. J Hepatol 2020;72:230-8.
82. Zhang X, Coker OO, Chu ES, et al. Dietary cholesterol drives fatty liver-associated liver cancer by modulating gut microbiota and metabolites. Gut 2021;70:761-74.
83. Castera L, Friedrich-Rust M, Loomba R. Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease. Gastroenterology 2019;156:1264-81.e4.
84. Wong VW, Chan WK, Chitturi S, et al. Asia-Pacific working party on non-alcoholic fatty liver disease guidelines 2017-part 1: definition, risk factors and assessment. J Gastroenterol Hepatol 2018;33:70-85.
85. Loomba R, Lim JK, Patton H, El-Serag HB. AGA clinical practice update on screening and surveillance for hepatocellular carcinoma in patients with nonalcoholic fatty liver disease: expert review. Gastroenterology 2020;158:1822-30.
86. Simmons O, Fetzer DT, Yokoo T, et al. Predictors of adequate ultrasound quality for hepatocellular carcinoma surveillance in patients with cirrhosis. Aliment Pharmacol Ther 2017;45:169-77.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Desjonqueres E, Gigante E. Hepatocellular carcinoma on the background of nonalcoholic fatty liver disease: epidemiological update. Hepatoma Res 2022;8:16. http://dx.doi.org/10.20517/2394-5079.2021.136
AMA Style
Desjonqueres E, Gigante E. Hepatocellular carcinoma on the background of nonalcoholic fatty liver disease: epidemiological update. Hepatoma Research. 2022; 8: 16. http://dx.doi.org/10.20517/2394-5079.2021.136
Chicago/Turabian Style
Desjonqueres, Elvire, Elia Gigante. 2022. "Hepatocellular carcinoma on the background of nonalcoholic fatty liver disease: epidemiological update" Hepatoma Research. 8: 16. http://dx.doi.org/10.20517/2394-5079.2021.136
ACS Style
Desjonqueres, E.; Gigante E. Hepatocellular carcinoma on the background of nonalcoholic fatty liver disease: epidemiological update. Hepatoma. Res. 2022, 8, 16. http://dx.doi.org/10.20517/2394-5079.2021.136
About This Article
Special Issue
Copyright
Data & Comments
Data

 Cite This Article 18 clicks
Cite This Article 18 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.