Microwave coagulation therapy: the future is quite rosy
To the editor
We read with great interest the review of Guan[1] on microwave coagulation therapy (MCT) of hepatocellular carcinoma (HCC), and we strongly agree with his conclusion that MCT has a great promise for future use, especially with further technical improvements.
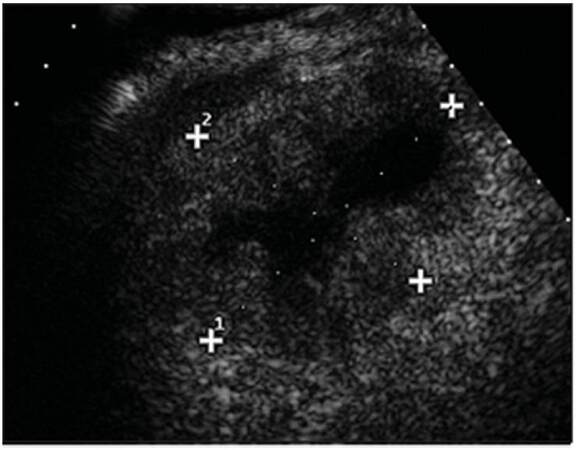
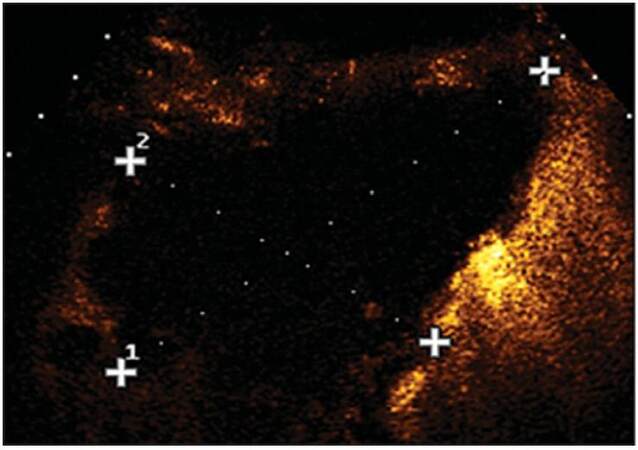
In this regard, one of the main limits of MCT [which discouraged its clinical application in many western countries in favor of radiofrequency ablation (RFA)] was the back heating effect, due to reflected waves along the coaxial line. Such a drawback imposed to use large antennas and to deliver energy for a short time, achieving small ablation areas and requiring multiple insertions even in the presence of small tumors.[2,3] Internally-cooled MCT partially reduced this problem, allowing for the increase of the ablation time and the amount of power that could be safely delivered.[4] The introduction into the distal portion of the antenna of a choke coil was proposed to reduce back heating effects. However, this remedy caused remarkable thickening of the antenna (9-10 gauge), making the device not suitable for percutaneous applications.[5] In the very last years, a miniaturized device for MW confinement has been developed (Mini Choke®), that enables to minimize back heating effects using slender MW antennas and allowing for percutaneous applications (AMICA MWA System, HS Hospital Service, Aprilia, Italy). In an experimental study, this system produced thermal lesions of 6.5 cm × 4.5 cm in ex vivo bovine liver by delivering 60 W for 10 min.[6] A randomized prospective comparison of MCT and RFA reported significantly larger coagulation areas in vivo with MCT than with internally-cooled RFA, using a 16-gauge internally-cooled, minichoked MCT antenna with a power output of 60-70 W and ablation time of 10 min.[7] Although energy delivery was underpowered with respect to the maximum power output of the system, MCT yielded ablation areas comparable to those previously reported by other authors who performed MCT using a power output of 100 W and a 14-gauge cooled shaft antenna without choke device.[8] As the minichoked MWA system can also use a 14-gauge antenna with a power output of 100 W, it is hypothesizable that ablation areas even larger than those obtained in the above-mentioned in vivo comparison between MCT and RFA could be achieved using the maximum power output. Indeed, we treated some HCCs and liver metastases measuring up to 7 cm × 6 cm, performing two insertions of a 14-gauge minichoked antenna and using a power output of 90 W for a total ablation time of 20 min, achieving coagulation areas measuring up to 10 cm × 7 cm [Figures 1 and 2].
Figure 1. Right intercostal contrast-enhanced sonogram showing a 7 cm × 6 cm colorectal metastasis of the right liver lobe
Figure 2. Right intercostal contrast-enhanced sonogram showing a 10 cm × 7 cm ablation area produced after two insertions of a 14-gauge internally-cooled, minichoked MW antenna using a power output of 90 W for a total ablation time of 20 min
Further randomized trials enrolling large series of patients are obviously needed to verify whether the superiority of MCT in obtaining larger ablation areas than RFA can translate into better long-term outcome and longer survival of patients with primary and secondary liver tumors, but it is indubitable that the technical improvement of MCT systems is already ongoing. According to the conclusion of the interesting review of Guan,[1] we believe that MCT is leaving its infancy and is running up to a quite rosy future.
Financial support and sponsorship
Nil.
Conflict of interest
There is no conflict of interest.
REFERENCES
2. Seki T, Wakabayashi M, Nakagawa T, Imamura M, Tamai T, Nishimura A, Yamashiki N, Okamura A, Inoue K. Percutaneous microwave coagulation therapy for patients with small hepatocellular carcinoma: comparison with percutaneous ethanol injection therapy. Cancer 1999;85:1694-702.
3. Horigome H, Nomura T, Saso K, Itoh M. Standards for selecting percutaneous ethanol injection therapy or percutaneous microwave coagulation therapy for solitary small hepatocellular carcinoma: consideration of local recurrence. Am J Gastroenterol 1999;94:1914-7.
4. Wang Y, Sun Y, Feng L, Gao Y, Ni X, Liang P. Internally cooled antenna for microwave ablation: results in ex vivo and in vivo porcine livers. Eur J Radiol 2008;67:357-61.
5. Ahmed M, Brace CL, Lee FT Jr, Goldberg SN. Principles of and advances in percutaneous ablation. Radiology 2011;258:351-69.
6. Cavagnaro M, Amabile C, Bernardi P, Pisa S, Tosoratti N. A minimally invasive antenna for microwave ablation therapies: design, performances, and experimental assessment. IEEE Trans Biomed Eng 2011;58:949-59.
7. Di Vece F, Tombesi P, Ermili F, Maraldi C, Sartori S. Coagulation areas produced by cool-tip radiofrequency ablation and microwave ablation using a device to decrease back-heating effects: a prospective pilot study. Cardiovasc Intervent Radiol 2014;37:723-9.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Tombesi P, Vece FD, Sartori S. Microwave coagulation therapy: the future is quite rosy. Hepatoma Res 2016;2:107-8. http://dx.doi.org/10.4103/2394-5079.170543
AMA Style
Tombesi P, Vece FD, Sartori S. Microwave coagulation therapy: the future is quite rosy. Hepatoma Research. 2016; 2: 107-8. http://dx.doi.org/10.4103/2394-5079.170543
Chicago/Turabian Style
Tombesi, Paola, Francesca Di Vece, Sergio Sartori. 2016. "Microwave coagulation therapy: the future is quite rosy" Hepatoma Research. 2: 107-8. http://dx.doi.org/10.4103/2394-5079.170543
ACS Style
Tombesi, P.; Vece FD.; Sartori S. Microwave coagulation therapy: the future is quite rosy. Hepatoma. Res. 2016, 2, 107-8. http://dx.doi.org/10.4103/2394-5079.170543
About This Article
Copyright
Author Biographies

Data & Comments
Data

 Cite This Article 2 clicks
Cite This Article 2 clicks











Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.